A nevus is a benign skin tumor, popularly called a mole or birthmark. The name comes from the Latin Naevus, because. the tumor consists of nevoid cells. Appearing on the human body as a result of environmental influences, such formations can be localized in any part of the body, not excluding the mucous membranes. Nevi can vary in shape and size, appear as a flat spot or pea, and their color varies from light to dark brown. The number of moles changes throughout life; they are almost never found in newborn children, but in adolescence they appear in almost everyone.
Symptoms of papillomatous nevus
Papillomatous nevus, unlike simple moles, has an irregular shape and protrudes above the skin. Depending on the pigmentation, it can match the color of the skin or have a brown, brown tint. Black nevi are very rare. Sometimes pigmented hair passes through the papillomatous nevus. Papillomatous nevi occur both single and multiple. Most often, nevi are localized on the head, neck, and face, but there may be cases where they are located in other places of the skin.
A characteristic feature of a papillomatous nevus is its slow but constant increase in size. From the beginning of development it is not noticeable, but as it grows it begins to cause discomfort to a person. Nevus on the head are often injured when combing hair. As a result, inflammation may occur.
Papillomatous nevus is a serious cosmetic defect; it causes inconvenience and psychological discomfort to its owner. In adolescents and people with a delicate mental structure, this situation can cause prolonged depression.
Publications in the media
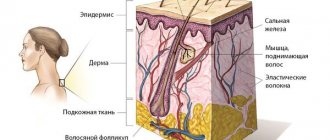
Nevi (moles, birthmarks) are hamartoma-like malformations of the skin that can develop both from elements of the epidermis and the dermis itself (connective tissue, vascular elements or melanocytes). Nevi are pigmented formations that usually protrude above the surface of the skin. Almost every person has moles; they can be congenital or occur throughout life, especially during puberty, in women during pregnancy, and hormonal dysfunctions. The clinical picture is characterized by extreme diversity in the number, size, morphological type and degree of pigmentation of individual elements - spots, nodules, plaques - up to subtotal damage to the skin with the so-called giant nevi. Large congenital nevi are considered to be elements >20 cm or occupying 2.5% of the body surface; they are considered a risk factor for malignancy.
• Epidermal nevi (warty or mole-like) are most often found at birth, although they can also develop in childhood (very rarely in adults). Externally they may be similar to papillomas (viral origin), but are usually represented by large linear plaques or an array of small papules. Epidermal nevi are often asymptomatic. Malignization is rare, with the exception of nevi of the sebaceous glands (basal cell carcinoma occurs in 5% of cases). Histologically they are characterized by acanthosis and hyperkeratosis. Nevus of the sebaceous glands is also characterized by the presence of a large number of sebaceous and apocrine glands. Cellular atypia is not observed. Treatment is mainly for cosmetic purposes. Preventive removal of sebaceous gland nevus is performed due to clinical manifestations (hair does not grow on it), and not the danger of malignancy.
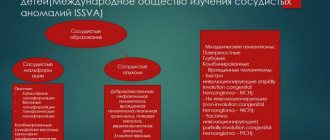
• Dermal nevi •• Connective tissue nevi are predominantly congenital and are often represented by dense, single papules and flesh-colored plaques. The number of hair follicles in them can be significant (“pigskin”). This variant of nevi is idiopathic and is not associated with other diseases, with the exception of “shagreen skin” in tuberous sclerosis. Histologically, they consist of dense conglomerates of collagen and elastic fibers. Prognostically safe and removed solely for cosmetic reasons •• Vascular nevi (hemangiomas) are vascular formations lined with endothelium, mainly capillary, but cavernous structures can also occur, especially in large nevi. Three clinical types are considered typical: strawberry nevus, cherry nevus and cavernous hemangioma. Strawberry nevus and cavernous hemangiomas more often undergo spontaneous regression, while cherry nevus continues to grow throughout life. Surgical treatment is carried out for cosmetic reasons, for functional disorders (localized in the conjunctival area, lips) or thrombosis of the cherry nevus (due to suspicion of malignancy) •• Melanocytic nevi are of the greatest clinical importance, given the need for differential diagnosis with melanoma •• Pathohistology. Nevus cells are located in the form of nested clusters of various sizes and configurations in the dermis, subepidermally and between cell complexes. Sometimes the accumulations become diffuse and are located very close to the epidermis along the basement membrane, and atrophic changes in the epidermis are noted. The cells are large, of various shapes and sizes, with a clearly visible nucleus, sometimes several hyperchromatic nuclei, arranged in the form of “rosettes” or lumpy clusters. In some elements, the shape of the cells is spindle-shaped, which makes the nevus resemble a neurofibroma. Pigment content may vary. In “young” nevi, the stromal component is weakly expressed; over time, the connective tissue stroma begins to predominate; such a nevus is considered “fibroepithelial.” Localization of nevus cells among basal keratinocytes and in the zone of the basement membrane without its disruption is characteristic of a border nevus, and in combination with the intradermal component - of a mixed nevus.
Clinical types of nevi • Basal cell nevus - a hereditary disease (109400, 601309, BCNS gene, 9q22.3, Â) - characterized by (usually benign) skin lesions of the eyelids, nose, cheeks, neck, upper jaw, looks like a flesh-colored papule, without signs erosion, histologically does not differ from basal cell carcinoma. • Verrucous nevus is a skin-colored (or darker) lesion of the epidermis similar to a wart, often linear, appearing at birth or in early childhood; can be of different sizes and localization, single or multiple “verrucous nevus. • Hairy nevus is a mole covered with a large amount of growing hair. • Giant pigmented nevus is a large congenital, with pronounced hair growth, pigmented nevus with a predominant localization on the lower extremities “pigmented hairy nevus” .
• A blue nevus is a wide-based papule or plaque of varying shades of gray-blue color. Histologically, clusters of process melanocytes with a high pigment content are found in the dermis, located parallel to the epidermis, which determines the optical effect of blueness when incident rays of the visible spectrum “Jadassohn-Tische nevus”. • Intradermal nevus - a nevus with localization of nests of melanocytes in the dermis, and not at the border between the epidermis and dermis. • Ito nevus - pigmentation of the skin area innervated by the lateral branches of the supraclavicular nerve and the lateral cutaneous nerve of the shoulder; nevus cells lying randomly in the dermis.
• Strawberry nevus - a small vascular nevus similar in size, shape and color to strawberries - a bright red solitary formation of spongy density. It is observed in 3% of newborns and often spontaneously obliterates by 6-7 years of age. « cavernous hemangioma « cavernoma « cavernous hemangioma. • Unilateral nevus is a congenital linear nevus, which is located along the nerve either on one side of the body or on part of a limb also on one side linear nevus. • Ota nevus (oculodermal melanosis) - skin pigmentation in the area of innervation of the trigeminal nerve and conjunctiva of the eye in the form of bluish-gray spots; occurs in Asia, more often in women. The treatment is cosmetic. • Nevus dark blue orbital-maxillary .
• Borderline nevus - a nevus consisting of nests of nevus cells near the basal layer, the border of the epidermis and dermis, appears as a small, slightly raised, flat, non-hairy, pigmented (dark brown or black) tumor epidermal nevus. • Acquired nevus is a melanocytic nevus that is not detected at first after birth, but appears in childhood or in adults. • Flaming nevus ( port wine stain) is a large, vascularized nevus with a purple coloration, usually located on the head and neck. Unlike other vascular nevi, in this case there is no proliferation of a large number of vascular elements, but an expansion of the normal number of skin vessels. As the size of the vessels progresses, protrusion appears and the color of the nevus changes from pink to purple-red. See also Sturge-Weber syndrome in the appendix to this article. • Sebaceous nevus (Jadassohn) - congenital hyperplasia of the sebaceous glands with papillary acanthosis of the epidermis. • With thick curly hair, nevi are congenital foci of growth of spirally twisted hair in the scalp “limited [symmetrical] allotrichia.
• Atypical nevus syndrome (ICD-10: D22 Melanoform nevus; *155600, #155601 [mutation of the CDKN2A cyclin-dependent kinase inhibitor 2A gene, OMIM 600160.0001]) is an inherited disease (Â)) of pronounced familial nature. Prevalence: in the USA up to 5% of the general population; in the late 90s, about 40 thousand familial cases and 4.6 million sporadic forms were registered. Synonym: dysplastic melanocytic nevus •• Clinical picture. Usually spotted elements, but there are papular, plaque-like elements with a central papule or micropapules, oval or irregular in shape, sometimes with processes, 5 mm in size or more, with a finely scalloped clear outline, of varying intensity of brown color (up to black), with an erythematous rim along the periphery •• Pathohistology. There are no generally accepted criteria for diagnosing dysplastic nevus. The architecture of a dysplastic nevus suggests uneven hyperplasia of the epidermal processes with hypertrophy of the terminal sections. Melanocyte cells of adjacent processes are often connected. Among epidermal melanocytes, a spectrum of cytological changes is observed: from moderate pleomorphism to obvious atypia. The pronounced degree of the latter can be interpreted as melanoma in situ. • Red-blue vesicular nevus syndrome (*112200, Â)). Blistering hemangiomas of the skin, especially the trunk and upper extremities, night pain, regional hyperhidrosis, bleeding gastrointestinal hemangiomas, angiomatous gigantism, cerebellar medulloblastoma.
• Mucosal spongy white nevus is a congenital keratosis of the mucous membranes, manifested by a thickened white spongy fold of the oral mucosa. • Vascular nevus - congenital uneven red coloring of the skin due to the proliferation of skin capillaries “vascular nevus” hemangioma. • Spitz nevus is a benign juvenile melanoma (see below Juvenile nevus). • Elastic Levandowski nevus - clusters of smooth or bumpy papules of ivory or flesh color, found symmetrically on the trunk and limbs “collagenous nevus”.
• Juvenile nevus •• Spindle cell and/or epithelioid cell nevus (juvenile melanoma, benign juvenile melanoma, Spitz nevus) is a benign melanocytic nevus, usually acquired, having a characteristic histological structure different from other types of melanocytic nevi. Initially it was believed that it occurs mainly in children, but it has now been shown that juvenile nevus is more common (up to 60%) in adults •• Clinical picture. Usually the exophytic formation is hemispherical, less often flat; dense elastic consistency, with clear boundaries; color - from light red to dark brown, sometimes black; the surface is smooth or papillomatous •• Pathohistology. According to its architectonics, a nevus can be borderline, mixed (most often), intradermal. According to the cellular composition, it can be spindle-shaped, epithelioid cellular, and more often mixed. The pigment content in melanocytes is variable. Characteristic is the presence of eosinophilic accumulations - fragments of the basement membrane (the so-called Camino bodies). Spindle-shaped melanocytes are elongated with an elongated nucleus and a large eosinophilic nucleolus. In the epidermis, melanocytes have long cytoplasmic processes and form large elliptical nests, the long axis of which is usually perpendicular to the skin surface. In the dermis, spindle cells are often located parallel to each other in the form of bundles or cords. Polygonal or round epithelioid cells with abundant fine-grained, reticulate or vacuolated cytoplasm. Giant multinucleated cells are often found.
Treatment is indicated for dysplastic, nodular and giant pigmented nevi due to their possible malignancy • Indications for excision of any pigmented formation •• Change in color, size, shape and consistency •• Pain syndrome •• Regional lymphadenopathy • Further therapy after excisional biopsy of a healthy area skin are prescribed based on the results of histological examination and localization of the formation.
ICD-10 • D22 Melanoform nevus • I78.1 Non-tumor nevus • Q82.5 Congenital non-tumor nevus
Application. Sturge-Weber syndrome (185300) is classified as phakomatoses, characterized by a triad: congenital cutaneous angioma (flaming nevus), usually along the trigeminal nerve, often unilateral; homolateral meningeal angioma with calcification and neurological signs; angiomas of the choroid, often with secondary glaucoma; in incomplete forms, any two or more signs are possible, sometimes with angiomas of a different localization “encephalotrigeminal angiomatosis” Sturge-Weber disease “nevoid amentia.”
Diagnosis of papillomatous nevus
For an accurate diagnosis, you need to consult an oncologist or dermatologist.
If a mole protrudes significantly beyond the skin, but does not cause discomfort, it should still be shown to a dermatologist. Accurate diagnosis of this type of skin formation is necessary in order to exclude melanoma and melanoma-dangerous nevi. Also, the type of tumor will help the doctor decide on treatment tactics. As a rule, a dermatologist will immediately distinguish a papillomatous nevus from an ordinary mole. Siascopic examination can be used for diagnosis. In difficult cases, a tumor biopsy, skin ultrasound and in-depth dermatoscopy are performed. In oncology, there are several types of nevi, depending on the size:
- small - up to 1.5 cm;
- medium - up to 10 cm;
- large - up to 20 cm;
- giant more than 20 cm.
A patient's risk of developing cancer directly depends on the size of the nevus.
Based on the place of their formation, nevi are divided as follows:
- epidermal - are an accumulation of melanocytes in the upper layers of the skin;
- intradermal - accumulation of melanocytes in the dermis;
- borderline - an accumulation of melanocytes between the upper layer of the skin and the dermis.
Hemangioma
Hemangioma is a benign tumor of blood vessels. It is a spot on the skin of red, raspberry or cherry color. May rise slightly above the surface of the skin. Sizes - from a pinhead to quite large (see photo).
Treatment of papillomatous nevus
Due to the fact that the nevus is constantly exposed to external factors, it can become damaged and then inflammation will begin, which can be easily recognized by soreness and redness. If during the diagnostic process doctors managed to completely exclude melanoma, dermatologists recommend removing the nevus with mandatory further histological examination of the formation.
Removal of papillomatous nevus can be carried out using a laser, cryodestruction, radio wave, electrocoagulation or surgical excision. Typically, all of the above operations are performed under local anesthesia.
Surgical operations
Large papillomatous nevus undergoes surgical excision. The application of small cosmetic stitches after the removal operation guarantees minimal cosmetic defects. The possibility of relapse is excluded, since along with the nevus, the doctor also captures part of the healthy tissue when removing it. Giant nevi are also treated surgically. They are rare, but the risk of developing cancer in them is very high. Treatment of giant pigmented nevus is carried out in stages, with the involvement of plastic surgeons for further cosmetic operations.
Currently, there is no method that can prevent the appearance of a nevus. The only thing that can be avoided is the transformation of a nevus into melanoma. To do this, you just need to make sure that the nevus is not injured. Under no circumstances should you engage in self-extraction and self-diagnosis of nevi, as this may lead to undesirable consequences. Do not neglect your health, and if a large mole appears or damages an existing one, consult a doctor immediately.