Dysplastic nevus - what is it?
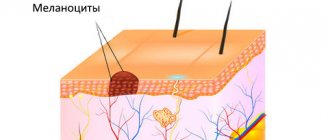
Like most moles in humans, a dysplastic (atypical) nevus is a pigmented nevus consisting of nevus cells. These cells are very similar to melanocytes. They also secrete the brown pigment “melanin”, but they differ in a number of characteristics that are not of fundamental importance to us.
It is important to note that dysplastic nevus is a histological diagnosis. This means that not all moles that look dysplastic in appearance will actually turn out to be dysplastic after removal and examination.
Methods for treating nevi
Treatment is allowed only in patients over 2 years of age. Therapy has 4 main directions:
- surgical removal;
- laser excision;
- cryodestruction;
- electrocoagulation.
As a rule, nevi that have grown deeply into the tissue are surgically removed. Giant neoplasms are removed in several stages, but the disadvantage of this method is the formation of scars at the site of the nevi.
Laser coagulation is used to remove dysplastic pigmented nevi and other clinical types of spots. The method allows removal of the formation without pain and without subsequent scarring.
Cryodestruction involves exposing the affected area of skin to very low temperatures. As a result, the altered cells die and are replaced by healthy ones. After cryodestruction, a small crust appears, which quickly disappears.
Electrocoagulation affects the nevus with high temperatures. Typically this method is used to remove small and medium-sized stains.
How to distinguish a regular mole from a dysplastic nevus?
Atypical nevi have a number of characteristic features that can occur either individually or in combination with each other.
| Round, symmetrical shape | Uneven edge and/or asymmetrical shape |
| Completely flat or completely raised above the skin | One part can be raised, the other flat (fried egg) |
| Uniform color or shades of brown | Black, red, brown at the same time |
| Size less than 6mm | Size over 6mm |
| Localization on any part of the body | Rarely located on the face |
diagnosis of pigmented nevus
- Finding out the history of the disease and visual examination of the pigment spot allows you to obtain up to 50% of the information.
- Dermatoscopy is performed in most developed clinics. The essence of the study is to view the nevus under a fluorescent microscope. Using this method, you can evaluate the surface of the nevus, the presence of microcracks, the color of individual parts, the condition of nearby skin, signs of inflammation, and more.
- Computer diagnostics of pigment spots is an expensive procedure and is not carried out everywhere. With its help, the diagnosis of one or another type of nevus is made with up to 90% confidence.
- A nevus biopsy is performed as a last resort and according to strict indications. It is better to carry out a targeted biopsy of an already removed formation followed by histological examination. This type of diagnosis is the most accurate.
How to distinguish a dysplastic nevus from melanoma?
A theoretically prepared reader, after reading the table, will exclaim: “You have now listed almost all the symptoms of melanoma!!! How can you tell them apart???” Unfortunately, a person without experience in diagnosing skin cancer, as a rule, cannot do this.
If you find moles on your skin with signs of dysplastic nevi, you need to see an oncologist. This doctor will examine them and also tell you about the signs of nevi turning into melanoma and the principles of monitoring such formations.
Stages of changes in nevi
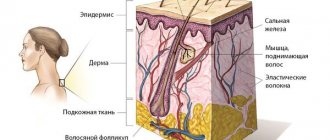
Melanocytic nevi , both acquired and congenital, are characterized by staged changes throughout life. The classic path of development includes 3 stages, which differ in the depth of the formation:
- a simple nevus or borderline nevus is a superficial flat brown spot;
- a complex or combined nevus is located deeper and looks like a brown spot or raised formation on the skin;
- An intradermal nevus is a light-colored, raised formation located deep in the skin.
Dysplastic nevus syndrome
Unfortunately, there is a syndrome that in Russian literature is often called nevus dysplastic syndrome (in foreign literature - FAMMM).
This disease has 2 diagnostic criteria
- the number of dysplastic nevi on the skin is more than 50
- melanoma in relatives
This disease may be associated with a mutation in the CDKN2A gene, which also increases the risk of developing pancreatic cancer
With this syndrome, the risk of developing melanoma, according to different authors, varies from 56 to 100%. The disease requires regular (once every few months) monitoring by an oncologist.
Causes of nevus
Pigmented nevi appear in utero, in other words, they are often congenital. Somewhere between 15 and 24 weeks of pregnancy, pigment cells migrate from the neuroectodermal tube to the superficial layers of the skin and form clusters of nocytes there, leading to the appearance of a birthmark. It is believed that such migration occurs under the influence of unfavorable factors affecting a pregnant woman. These include: infections (especially viral ones), taking certain medications, excessive insolation, radiation, and the effects of toxic substances. Genetic predisposition is also no exception.
With age, new nevi may appear, however, there is an opinion that this is only a manifestation of long-existing skin changes that arose in utero. Pregnancy, menopause, allergic and autoimmune diseases, exposure to harmful production factors, and much more can push the body to the appearance of new moles.
What to do if there are dysplastic nevi on the skin?
There is an opinion on the Internet that “all dysplastic nevi should be removed.” I consider this point of view incorrect for the following reasons:
- A very small percentage of nevi that look atypical upon examination turn out to be so upon histological examination.
- An even smaller proportion (0.0001%) of truly dysplastic nevi have a chance of becoming melanoma
- Skin melanoma can develop not from a nevus, but against the background of unchanged skin.
In this regard, for people who have dysplastic nevi, I usually recommend the following:
- Regular self-examination once a month with measurement of existing atypical nevi using a ruler. Optimally - with photographic recording of the result
- Examination by an oncologist once every 6 or 12 months. The frequency depends on the number of nevi.
- It makes sense to remove elements that are difficult to access for self-examination, as well as those that have changed in a short time
- Protect skin from the sun
- Gallery
- News
- Reviews
- Vacancies
- Licenses
- Insurance partners
- Controlling organizations
- Schedule for receiving citizens for personal requests
- What you need to know about coronavirus infection?
- Rules for patients
- Online consultation with a doctor
- Preparing for research
- to corporative clients
- Documentation
Dysplastic nevus is one of the types of flat pigmented skin formations, which are more often called moles.
Patients, and many doctors, mistakenly believe that all flat pigmented formations are benign and do not pay attention to them. However, it is known that dysplastic nevi can transform into melanoma. The transformation process occurs gradually as lentiginous melanocytic dysplasia (LMD) develops from grade 1 to grade 3.
This type of formation deserves the closest attention among all types, since there is a very high risk of their malignancy with transition to the most malignant tumor - melanoma. The term dysplastic itself means that it is a nevus that is not similar in external and internal characteristics to typical moles. Dysplastic nevus, which occurs in 5%-9% of the white population, has recently attracted the attention of researchers, as it may be a precursor to superficial spreading melanoma: it is found in almost all patients with hereditary melanoma and in 30–50% of patients with sporadic melanoma . A dysplastic nevus can occur on intact skin or be a component of a complex noncellular nevus.
Clinically, dysplastic nevus is similar to borderline nevus, but there are also differences. Thus, a dysplastic nevus is an irregularly shaped spot, while a borderline nevus has a regular shape - round or oval. The color of a dysplastic nevus is often heterogeneous, with areas of dark pigment, while a borderline nevus is characterized by a uniform color, the color of both nevi varies from light brown to dark brown. Often, a pinpoint formation resembling a target is noted in the center of a dysplastic nevus. When a dysplastic and mixed nevus is combined, there is a picture of a “fried egg” with a raised yolk in the center.
In our observations, dysplastic nevi were found in 5% - 10% of patients who consulted a surgeon or oncologist for various diseases. In some, the nevi were single - from 3 to 10 formations, in others - multiple - from 50 to 100 or more. Observing patients with multiple dysplastic nevi, we identified 2 types of these formations.
In the first type - there were fewer of these patients - dysplastic nevi appeared in childhood and adolescence, were often hereditary, but these patients did not report melanoma in relatives. Carriers of nevi were, as a rule, white-skinned, poorly tanned, with blond or red hair and light eyes. Dysplastic nevi of this type were large - 0.5 - 1.0 cm in diameter, located on open and closed areas of the body (buttocks, lower abdomen), and were often combined with papillomatous nevi. The color of nevi in the same patient could vary from pink to dark brown, sometimes a variegated color was observed: dark areas on a pink or light brown background. This pattern of nevi has been described as “dysplastic nevus syndrome.” After puberty, new nevi did not appear in this group of patients. This fact can be attributed to the fact that white-skinned people limited their exposure to the sun, as they quickly burned, and were also informed about the possible appearance of new “moles” as a result of exposure to ultraviolet radiation.
In the second type, dysplastic nevi were rare in adolescence; most nevi appeared in adulthood and were associated with frequent and prolonged exposure to the sun while vacationing in southern latitudes. Dysplastic nevi of this type were small - from 0.1 to 0.4 cm in diameter, regular rounded in shape, uniform in color, combined with multiple freckles in young patients and pigment spots of the “Dubreuil’s melanosis” type in older patients. In white-skinned patients with skin phototype 1 - 2, the nevi were light brown, in others they were brown or dark brown. The density of nevi was higher on sun-exposed areas of the body: the face, forearms, outer surface of the shoulders, upper half of the back and chest wall (like a “wide neckline”). All this indicates some similarity between dysplastic nevi of the second type and Dubreuil’s melanosis, which is a proliferation of melanocytes in the basal layer of the epidermis in individuals with skin phototype 1 - 2 under the influence of repeated sunburn.
According to our observations, the most important sign of progression of dysplastic nevus is:
- The appearance of pigment formation on unchanged skin and its further growth over several months or years in persons over 18 years of age , i.e. in adulthood.
- Changes in the last 3-5 years of a long-existing nevus may indicate the progression of a dysplastic nevus, which is combined with a borderline or mixed nevus.
- An important sign of a progressive dysplastic nevus is a very dark color (almost black), or uneven coloration of the formation with areas of dark brown or black.
- The irregular shape of the nevus may be little noticeable with a small size of the progressive dysplastic nevus , at the same time it can also be observed in a long-existing noncellular nevus - borderline or mixed.
Excision of dysplastic nevus
Excision of the nevus (excisional biopsy) should be performed under local anesthesia, 0.4–1.0 cm from the visible boundaries, with subcutaneous tissue. Histological examination of a removed nevus should be carried out by a pathologist with experience in the study of melanocytic formations. Progressive dysplastic nevi require excision for prevention purposes, as well as early diagnosis of cutaneous melanoma . When melanoma is detected, the question of the need for reoperation - excision of the postoperative scar - is decided depending on the thickness of the tumor, determined by histological examination. According to foreign authors, as well as WHO recommendations, an adequate deviation from the boundaries of the formation for in-situ melanoma is 0.2 - 0.5 cm, for invasive melanoma with a thickness of less than 1.5 mm - 1.0 cm.
During removals carried out in the department of surgery from June 2009 to April 2014, of all removed pigmented formations, the clinical diagnosis of “dysplastic nevus” was confirmed morphologically in 76% of cases, i.e. Histological examination of these formations revealed structures of lentiginous melanocytic dysplasia (LMD). In 2.4% of cases, melanoma was detected that developed against the background of LMD ; in other cases, other types of nevi were confirmed (intradermal, mixed nevus, nevus of the sebaceous glands). In our clinical cases, patients with diagnosed melanoma did not require reoperation.
Foreign authors recommend removing dysplastic nevi 0.6 cm or more; according to our research, smaller nevi - 0.4 - 0.5 cm in diameter - can also be removed. In our practice, melanoma in one case measured 0.5 x 0.4 cm, in another - 0.5 cm.
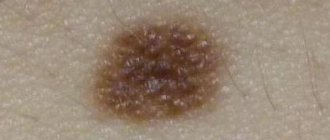
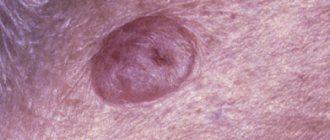
Photos 1 and 2 show dysplastic nevi with signs of progression.
Photo 1 shows a nevus of the gluteal region measuring 0.5 x 0.4 cm in a 29-year-old patient with skin phototype 1. The nevus, according to the patient, appeared 7 months ago in the form of a punctate formation, which gradually increased (a sign of progression) . No other pigmented nevi or freckles were found on the body. Histological examination: lentiginous pigmented nevus with severe (grade 3) melanocytic lentiginous dysplasia.
Photo 2 shows a nevus of the chest wall in a 27-year-old patient , 0.3 cm in diameter, round in shape, which darkened after staying in the south (a sign of progression) . Histological examination - mixed dysplastic pigmented nevus with severe (grade 3) melanocytic lentiginous dysplasia.
If the patient refuses surgery or in the absence of obvious signs of progression of the dysplastic nevus, the nevus should be re-examined by a doctor after 6 months. If there are changes in the nevus over the past period, surgery is recommended; if there are no changes, further observation after 6 months.
Patients with dysplastic nevi need:
- avoid prolonged exposure to direct sunlight,
- protect the skin with clothing,
- apply sunscreen.
The material was prepared based on the article: “Tactics for managing a patient with a dysplastic nevus” - O.A. Romanova, N.G. Artemyeva, E.A. Yagubova, I.M. Rudakova, V.N. Marycheva, A.A. Veshchevaylov . Clinical dermatology and venereology No. 2, 2015.
Services and prices
Histological examination of skin biopsy material
1,650 rub.
Appointment with a dermatovenerologist, therapeutic and diagnostic, primary, outpatient
2,000 rub.
Appointment with a dermatovenerologist, therapeutic and diagnostic, repeat, outpatient
1,800 rub.
Appointment with an oncologist, treatment and diagnostic, primary, outpatient
2,000 rub.
Appointment with an oncologist, therapeutic and diagnostic, repeated, outpatient
1,800 rub.
Appointment with a surgeon LD, PERV, AMB
2,000 rub.
Appointment with a surgeon, candidate of medical sciences, primary, outpatient
2,500 rub.
Removal of benign formations with a diameter of up to 5 mm using the molecular resonance surgical device VESALIUS LX 80 (with anesthesia and bandage)
2,500 rub.
Removal of a benign tumor with a diameter of more than 5 mm using a molecular resonance surgical device VESALIUS LX 80 (with anesthesia and bandage)
3,100 rub.
Isaeva Galina Ivanovna Oncologist Work experience: 19 years
Romanova Olga Aleksandrovna Oncologist (mammologist) Work experience: 62 years
Artemyeva Nadezhda Georgievna Head of department, surgeon, phlebologist Doctor of the highest category Work experience: 43 years
Bezlepko Marina Gennadievna Oncologist Work experience: 13 years