All people have moles on their bodies.
Among them there may be a birthmark that looks like a wart, called a warty nevus.
The danger of such a neoplasm is that it is capable of degeneration into a malignant form.
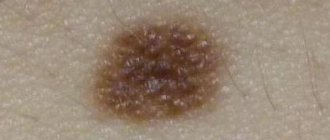
A warty (verrucous) nevus can be recognized by the presence of a bumpy surface.
The mole looks like a head of cabbage or has the appearance of a garland.
Nevus is dangerous, since such neoplasms often degenerate into a cancerous tumor.
A mole may appear some time after the baby is born, and sometimes it forms much later.
- Initially, a convex formation appears on the surface of the child’s skin. As it grows, the formation darkens and becomes brown or yellowish.
- As the child grows, the mole also becomes more noticeable, but there is no growth in width. The size of the nevus increases due to the proliferation of epithelial tissue that it affects.
- Over time, the surface of the neoplasm becomes keratinized and the mole becomes convex. As a result of injury to the upper layer, the neoplasm becomes larger.
In most cases, moles are not dangerous, but sometimes they become so as a result of degeneration into a malignant form.
Why does a warty nevus appear?
Scientists have come to the conclusion that the formation of moles begins at the embryonic stage of development.
Factors that provoke their formation in humans are:
- imbalance of female sex hormones in a woman during pregnancy
- the presence of infectious pathologies during pregnancy
- the influence of unfavorable environmental factors on a woman’s body during pregnancy
- hereditary factors
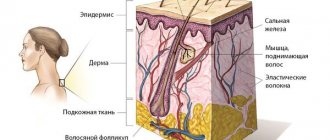
As a result of these reasons, the development process of melanoblasts, from which melanocytes are formed, is disrupted.
Melanocytes, concentrating in certain areas of the skin, turn into nevocytes.
Their difference from melanocytes is that they do not have processes that contribute to the spread of pigment.
Causes of moles
Most moles form in childhood and adolescence. Heredity and genetic predisposition play a key role. In adulthood, the appearance of new formations is facilitated by external and endogenous factors. The most important is hyperinsolation - regular and prolonged exposure of the skin to ultraviolet radiation.
Ultraviolet light is the main catalyst for the formation of melanin pigment in skin cells, and it is melanin that determines the color of the entire skin and its elements. The appearance of a black mole may be a consequence of too frequent and long exposure to the sun. Fans of artificial tanning are at risk, since solarium lamps are a source of intense ultraviolet radiation.
Changes in hormonal balance can contribute to the appearance of new nevi. For women, a risk factor is ovarian dysfunction (imbalance of sex hormones). Changes in hormonal levels can be triggered by taking oral contraceptives and hormone replacement therapy during menopause. The formation of black moles is possible during pregnancy and lactation.
Can a nevus turn into cancer?
A birthmark that forms in the upper layer of the skin poses a risk of degeneration.
Malignancy of a warty nevus can occur with repeated damage.
Please note the following changes:
- mole color change
- hair loss on a mole
- change in size towards larger tumors
- appearance of asymmetry
- presence of discharge from the nevus
- uneven edges
If at least one of the signs appears, you should immediately visit a doctor.
Types of warty nevus
There are localized forms of nevus manifestation or systemic (verrucous).
Localized - most moles are found in this form.
Signs of its manifestation:
- The diameter of the neoplasm does not exceed 1 cm.
- elements appear separately or are located so close that they can merge
- localization zone is clearly limited
- the keratinized surface of the nevus often has cracks
- moles are dark brown or maroon in color. In very rare cases, nevi are light brown or light pink in color.
- the area affected by moles is often devoid of hair
Systemic form of the disease - the incidence of pathology is approximately 20% of cases.
A distinctive feature of a nevus is the presence of a “garland” of neoplasms.
Such elements are located at close distances relative to each other and “stretch” along the surface of the skin along the entire body.
This form of nevus has a number of features:
- the elements spread along large vessels, and they can also be in different places of the body
- The surface layer of moles may differ in shade. Elements may have different color intensities
- the length of one garland can reach up to 20 cm.
- When feeling the moles, it is noted that they have a dense structure
- the surface of each mole is lumpy and tortuous. As a person ages, these symptoms become more pronounced.
Each type of warty mole can be frequently injured.
Types of epidermal nevi
There are several clinical types of epidermal nevi. This classification is not definitive, since epidermal moles can be hard, linear and inflamed at the same time.
Soft papillary nevus of the epidermis . This is most often a small flesh-colored or gray formation with a soft, velvety surface. Individual papules forming clusters resemble senile warts.
Hard papillary nevus.
Unilateral, segmented, most often located on the trunk and limbs. These are tall or flat, raised discolorations of normal skin, light or dark brown, with a papillary surface.
Inflammatory linear verrucous epidermal nevus.
This is a special form of epidermal nevus with inflammation and severe itching. ILVEN may worsen and disappear, especially in the form of psoriasis-like psoriasis.
According to the conclusions of the study. Altman and Mehregan, diagnostic criteria for such moles include a number of features:
- early onset is noted - in 75% of cases before 5 years,
- more common in females (4 times more often);
- frequent localization on the left lower limb and buttocks;
- itching is usually present;
- histopathological appearance resembling psoriasis - a characteristic pattern of parakeratotic areas with visible psoriasis-like epidermal hyperplasia, mild spongy edema and exocytosis of lymphocytes;
- Such nevi have no tendency to spontaneous regression and resistance to treatment.
The lesions are linear, pruritic, erythematous lesions with a flaking surface and may resemble psoriasis lesions with a linear pattern. They are distinguished from psoriasis by the absence of Munroe microcirculation and the lack of epidermal involucrin expression in ILVEN. The connection with psoriasis is confirmed by the participation of the cytokines IL-6, IL-1, TNF-alpha, ICAM-1 in the pathogenesis.
Horny nevus (nevus corniculatus)
. This is the rarest form of epidermal nevus. The clinical picture shows very intense keratosis with the formation of thick papillary growths and filamentous formations. Histopathological examination shows foci of acantholysis with depressions in the epidermis filled with dense keratin.
Pediatric epidermal nevus.
This variety is characterized by congenital hemidysplasia, unilateral ichthyosis and limb defects. All of these disorders can occur, but it can only be the cutaneous form. The lesions are located unilaterally and do not extend beyond the midline of the body, with the most common lesions being the flexor folds. They have the character of erythematous lesions covered with yellow hyperkeratotic scales and sometimes with horny plugs. This type of mole occurs only in women because the gene responsible for the condition is located on the X chromosome.
Epidermal nevus syndrome, which is a combination of epidermal nevus with other developmental defects, has been clinically identified.
There are 4 clinical variants of the syndrome (Michalovsky classification):
- four-symptom form - lesions of the skin, bones, nerves and eyes.
- three-symptomatic form - skin, bone and nervous changes.
- two-symptomatic form - skin and bone changes.
- monosymptomatic form - the presence of a linear papillary epidermal nevus.
Characteristic manifestations of verrucous nevus
The neoplasms rise above the skin by 2 cm, but sometimes they can be higher.
Moles look like a cluster of a large number of papilloma-like growths, which are located very close to each other and can merge into a single whole.
The surface of the new growths is slightly rough and quite dense.
The color of verrucous nevus varies from flesh-colored to dark brown.
Growths can appear on any part of the skin surface.
Both single neoplasms and large numbers can be observed, including they can be fused and have an individual shape, size and color.
Verrucous nevus is characterized by the presence of elements on one side of the body (right or left).
When located on the extremities, the localization of neoplasms is noted in the area of large vessels and nerve bundles.
Keratotic nevus grows very slowly, possibly the growth of new elements.
An increase in the size of moles is more often observed in the longitudinal direction than in the transverse direction.
The presence of moles does not cause discomfort, they do not cause pain or itching, and do not interfere with any movements.
Their presence on the body has a pronounced cosmetic disadvantage, especially if they are located on open areas of the body or on the face.
Symptoms of nevus of Ota
Nevus of Ota is characterized by black-bluish or dark blue pigmentation of the skin of the temple, cheekbone, lower eyelid, cheek, and upper jaw. The localization of the spots is one-sided, less often both parts of the face are affected. Pigmentation can be single (one spot) or multiple (several spots). The skin is evenly colored. True, there are nevi with varying color intensities. Pigmentation may be subtle or bright blue. In any case, pigmentation is the first symptom of nevus of Ota.
Quite often, this nevus causes pigmentation of the iris, conjunctiva of the eyes and sclera, and may have a brown or bluish tint. In addition, there are cases when pigmentation spreads to the larynx, lips and even nose. The mucous membrane of the throat and palate also suffers.
The nevus is localized in the zone of innervation of the trigeminal nerve (I and II branches). There are not isolated cases when pigmentation can spread to the structures of the eye, but nevus of Ota does not cause neurological or visual disturbances. Thus, visual function does not suffer from this disease, only the face becomes covered with a pigment layer.
A person can “get” nevus of Ota immediately at birth. The disease can also manifest itself in early childhood and puberty. Nevus Ota will accompany a person throughout his life. However, it is known that the Mongolian type of spots disappears after some time.
Nevus of Ota very rarely degenerates into a malignant formation. This process is accompanied by changes in the area of the nevus:
- its color darkens or lightens;
- the borders of the nevus turn red;
- color unevenness is observed;
- bumps, erosions or cracks appear on its surface;
- the outline is blurred and the like.
Diagnosis of keratotic nevus
Only a specialist can identify the presence of a warty nevus.
Based on external data and a conversation with the patient, the doctor can make a preliminary diagnosis.
For a more accurate diagnosis, laboratory tests will be required.
When examining a nevus, the doctor pays attention to the presence of the following features:
- coloring of moles
- size of tumors
- Locations of birthmarks
- shape of moles
- absence or presence of hair on the surface of the neoplasm
To confirm the diagnosis, laboratory tests are performed:
- oncocytology. A scraping is taken from the surface of the nevus. The disadvantage of the technique may be a traumatic factor, which can provoke the development of complications such as infection or degeneration into melanoma. Therefore, this study is prescribed for those patients whose moles have been traumatized;
- Lumenescence microscopy technique. Its essence is to apply a special composition to the neoplasm, after which the birthmark is examined under a microscope. This research method is considered to be the safest, since the nevus is not injured during the procedure;
- conducting a computed tomogram , which allows you to examine the internal structure of moles using x-rays;
- blood tests . The blood is examined for tumor markers - specific proteins that are produced when the body is prone to cancer;
- histology . A piece of tissue is taken for examination. The resulting biomaterial is subjected to histological examination for malignancy of the nevus. This technique is informative enough to confirm the development of a malignant process.
Diagnosis - histopathological features of linear nevi
There is considerable variability in histopathological studies. The most common manifestations:
- hyperkeratosis;
- acanthosis;
- papillomatosis.
Some moles may exhibit acantholysis and dyskeratosis, resembling Darier's disease.
Sometimes you can find a picture of epidermolysis with hyperkeratosis, reminiscent of congenital bullous erythroderma ichthyosis. In these cases, mutations in the keratin 1 or 10 genes are found.
Diagnosis of nevus
Treatment of warty nevus
The basis of treatment for keratotic nevus is its removal using one of the most suitable methods.
The choice of method depends on the location of the warty nevus, its shape, and size.
The specialist decides which destruction method will be most effective.
To get rid of the manifestations of skin defects, the following techniques can be used:
- use of liquid nitrogen (cryotherapy)
- application of electric current (electrocoagulation)
- removal by radio waves (radiotherapy)
- destruction with a laser beam (laser therapy)
How to remove a warty nevus
Removal of a verrucous nevus is carried out using one of the following methods.
Surgical excision of moles is a classic method of ridding a patient of skin tumors.
After anesthesia and antiseptic treatment of the skin and surface of the nevus, it is cut out with a scalpel.
Then the wound is treated with a disinfectant and a sterile gauze bandage is applied.
This technique has negative aspects: infection of the wound surface and the formation of a postoperative scar are possible.
Removal of a nevus using radio wave radiation - this technique has many advantages:
- the ability to control the depth of exposure to radio waves, which avoids damage to healthy tissue around the tumor
- absence of bleeding due to their coagulation
- the procedure is painless
- the procedure is carried out very quickly
- radio waves can be used on any area of the skin
- There are no negative consequences after surgery
Laser therapy is one of the most common.
The laser beam can be used for keratotic moles on the scalp, as well as in the facial area.
Benefits of using laser:
- it is impossible for infection to penetrate at the site of exposure
- Coagulation of the wound eliminates the development of bleeding
- after removing the growth, a crust remains
- the risk of scarring is minimal
Removing nevus with liquid nitrogen: the use of low temperatures allows you to remove small tumors.
The procedure is painless.
Pain appears some time after exposure to nitrogen.
A disadvantage of the technique is also the need for repeated sessions, since the technique does not allow accurately calculating the time of exposure of the pathological tissue to nitrogen.
Electrocoagulation method - high frequency currents are used for treatment.
Before removal, the doctor administers local anesthesia.
As a result of exposure to electric current, a crust forms at the site of removal, which protects the wound from infection.
Treatment of epidermal moles
Epidermal moles persist throughout life, do not tend to disappear spontaneously and are primarily a cosmetic problem, especially on the skin of the face and neck. These are benign formations, although there are risks of developing cancer. A case of squamous cell carcinoma inside a nevus has been described in the literature. Treatment of epidermal moles is necessary for cosmetic reasons.
Treatment uses many different methods, varying in effectiveness and availability. When treating epidermal nevi, the following is used:
- surgical removal of the lesion;
- electrocoagulation;
- cryotherapy;
- dermabrasion;
- CO 2 laser;
- dye laser;
- tretinoin;
- 5-fluorouracil;
- acitretin;
- calcipotriol;
- dithranol;
- podophyllin;
- keratolytic drugs.
Conservative methods fail to achieve complete recovery, and scars remain after surgical removal of the lesion. The mechanism of action of individual methods is not always fully understood. For example, calcipotriol can affect the production and function of cytokines and normalize the differentiation of epidermal cells, 5-fluorouracil has an antiproliferative effect.
Some of the treatments that were used in the past are now only of historical significance.
According to many scientists, the most effective method of treating linear lesions in a small area is to remove the nevus by surgical excision; however, when completely removing large lesions, it is necessary to cover the defect with a free skin graft, which is often associated with the formation of an unaesthetic scar.
The effect of laser on moles
Features of care for verrucous nevus
If elements of a wart nevus are found on a patient’s body, doctors suggest removing it to remove the cosmetic defect.
If the patient for some reason does not want or cannot do this, then he must follow a number of rules that will help avoid the development of complications.
The basic rules are as follows:
- Eliminate factors that may cause overheating of moles. Prohibited: visiting saunas, baths, spa treatments.
- In the warm season, avoid being under the rays of the sun during the hours of its greatest activity: after 10 a.m. and before 4 p.m. Avoid visiting the solarium. It has been proven that protective agents cannot prevent the development of melanoma;
- Before taking hormonal medications, you should first consult with a specialist.
- Monitor the condition of the nevus elements and consult a doctor at the first symptoms of malignancy of moles.
You should pay attention to the following changes:
- accelerated nevus growth
- the appearance of unpleasant sensations that were not there before: pain, itching, burning, etc.
- change in the color of the neoplasm, it may become multi-colored
- appearance of peeling
- formation of cracks on the nevus
- hair loss
- asymmetrical growth, torn edges
- acquisition of granularity by a mole
- formation of outgrowths
- the appearance of discharge of various types
If at least one of the above symptoms appears, you should immediately consult a doctor.
If treatment turns out to be timely, then birthmarks will not pose a danger to a person in terms of malignancy.
And modern treatment methods will eliminate the presence of discomfort, both physical and cosmetic.
It is important to understand that self-medication can cause irreparable harm to health.
Removal of tumors should only take place in a medical facility and be carried out by a specialist.
Treatment of papillomatous nevus
Due to the fact that the nevus is constantly exposed to external factors, it can become damaged and then inflammation will begin, which can be easily recognized by soreness and redness. If during the diagnostic process doctors managed to completely exclude melanoma, dermatologists recommend removing the nevus with mandatory further histological examination of the formation.
Removal of papillomatous nevus can be carried out using a laser, cryodestruction, radio wave, electrocoagulation or surgical excision. Typically, all of the above operations are performed under local anesthesia.
Why is a warty nevus dangerous?
This type of mole among other nevi is the safest.
A certain group of factors can contribute to its degeneration.
The possibility of infection due to injury to a mole can provoke the development of an inflammatory process.
If a keratotic nevus is localized on the head or in another area of increased risk of injury, they should be removed as quickly as possible after their formation.
In some cases, manifestations of a systemic warty neoplasm can serve as a sign of hydrocephalus and other lesions of the nervous system, as well as melanoma.
In this case, therapy should be carried out simultaneously by several specialists: oncologist, neurologist and dermatologist.
Diagnostics
Detection of nevi, as a rule, occurs accidentally during ophthalmoscopy of the fundus. For a final diagnosis, their dynamic observation with regular examinations of the fundus, including examinations with color filters, is necessary. Thus, a choroidal nevus becomes clearly visible in red light, and when examined in green light, the nevus “disappears.” At the same time, only changes in the layers of the retina, which are characteristic of a progressive nevus, remain visible. Ultrasound examination, in some cases, can sometimes reveal the protrusion of the formation. With fluorescein angiography (examination of the fundus vessels using a contrast agent - fluorescein), the presence of stationary nevi is indicated by the absence of changes in the vessels surrounding the choroid. With a progressive nevus, fluorescein angiography detects the leakage of fluorescein through the walls of the vessels adjacent to the nevus.
Preventive measures for warty nevus
Verrucous nevus can provoke the development of oncological pathology.
But with proper prevention it is possible to avoid complications.
Prevention of complications is as follows:
- eliminating the possibility of injury to neoplasms
- Seeing a doctor for excision of growths
- you need to forget forever about saunas and solariums. Even the use of sunscreen cosmetics cannot protect against the development of melanoma
- in hot weather, avoid going outside to prevent overheating of tumors
- stay indoors after 10 a.m. and before 4 p.m.
- If at least one of the signs of malignancy appears, immediately go to the doctor
- Regular visits to a specialist to monitor moles
Melanocytic nevi
The article presents options, clinical manifestations, clinical features, and diagnostic criteria for various types of melanocytic nevi.
The increased attention of doctors of all specialties to melanocytic nevi (MN) is explained by late diagnosis and poor prognosis of melanoma developing against them - one of the most malignant human tumors. Making up less than 10% of the structure of malignant skin neoplasms (MSN), melanoma is responsible for 80% of deaths in the entire group of MNS /1/. On the other hand, timely treatment of melanoma (at the stage of “horizontal” growth) allows patients to achieve a 10-year disease-free period of life in 90% of cases /7/.
It is known that melanoma occurs in approximately 50% of cases against the background of MN, which may be due to a common genetic defect - loss of heterozygosity in the 9p21 locus of chromosome /16/ with a mutation in the nRAS oncogene /20/ in both melanoma tissue and MN, against the background which it developed.
The most important factor in the development of melanoma against the background of MN is exposure of human skin to an excessive dose of UVR, which leads not only to damage to keratinocytes and melanocytes, but also to immunosuppression, caused primarily by the suppression of NK cells. In addition, risk factors for the development of melanoma are: skin phenotype I-II (proneness to sunburn of the skin, red hair, blue eyes, fair skin), 3 or more episodes of sunburn of the skin during life, the presence of freckles and lentigo or 3 or more atypical MN, familial cases of melanoma in close relatives /1/.
MNs are observed in ¾ of Caucasians /18/ and are benign tumors of the melanogenic system. Only some of them transform into melanoma (melanoma-dangerous MN) or are a marker of an increased risk of its development. /4,11,12,19/. Identifying them in order to prevent the development of melanoma is extremely important for doctors of all specialties.
The vast majority of MNs are acquired. They are divided into regular and special types.
Among common MNs, borderline, complex (epidermal-dermal) and intradermal forms are distinguished /15)/. They arise after the birth of a child and have characteristic dynamics: first, due to the proliferation of nevus cells along the border of the epidermis and dermis, the formation of borderline MN occurs; over time, nevus cells move into the dermis, forming mixed MN; the borderline component may disappear with age, leaving only the dermal (intradermal MN) component /3, 5, 6, 9/. The evolution of MN is associated with the phases of melanocyte involution: melanocyte - nevus cell - fibrous tissue /10/.
Clinically, borderline MN is manifested by a uniformly pigmented (from light brown to dark brown) spot with a diameter of 1-5 mm, round or oval in shape with a smooth surface and clear boundaries, located on any part of the skin and existing until approximately 35 years of age. Mixed MN is a pigmented papule, sometimes with papillomatosis, rarely reaching 1 cm in diameter. Intradermal MN is characterized by a dome-shaped or papillomatous papule, which in shape can resemble a blackberry (Fig. 1.), have a stalk or the shape of a mollusc-shaped element on a broad base (Fig. 2); its surface is covered with hair, its diameter rarely exceeds 1 cm, and its color varies from light brown to black. Rarely, depigmented MN with a whitish or pink-red color is found.
Rice. 1. Intradermal melanocytic nevus in the form of a blackberry.
Rice. 2. Intradermal melanocytic nevus mollusciform.
The dependence of the clinical picture of ordinary MNs on the localization and location of nevus cells in them was noted. Thus, on the palms and soles, the complex and intradermal MN (due to the large thickness of the stratum corneum) do not rise above the skin level; MNs raised above the skin level have a pronounced intradermal nevus component, and flat ones have a borderline component; The more the MN is raised above the skin level, the less pigmented it is.
Conventional MNs grow in proportion to the growth of the human body; after birth, their number increases, reaching a maximum during puberty, and after 50 years it gradually decreases, and by 7-9 decades of life they usually disappear. The regression of conventional MN is due to the degeneration of the cells that form it with their gradual replacement by fibrous and adipose tissue /10,24/. Sudden regression of such MNs occurs very rarely /29/.
The idea that melanoma-dangerous MN should include borderline and mixed forms (as those that retain a borderline component in their structure, including those localized in the area of the palms and soles, external genitalia, and nail bed) has now been revised. Thus, MN of the palms and soles, accounting for 4-9% of all MN, is currently not classified as melanoma-dangerous due to the fact that only dysplastic nevi of this localization transform into melanoma /17/. MN of the nail bed, the so-called longitudinal (linear) melanonychia in the form of pigmented lines running along the nail plate, can be not only borderline, mixed MN or acral-lentiginous melanoma, but also, often, the so-called “melanotic spot” (formed by increased melanin content in the cells of the basal layer of the epidermis without increasing the number of melanocytes) / 28 /. Although subungual melanoma occurs not only in adults but also in children, longitudinal melanonychia in children is almost always a benign process /21/.
Conventional MNs of the external genitalia are more often observed in young women in the area of the vulva and perineum, less often in the area of the male genital organs, but atypical histological signs are found in them extremely rarely (in 0.02% of cases) /27/. On the other hand, convincing evidence has been obtained that melanoma can develop both in the tissue of the intradermal MN and directly beneath it /30/.
Due to the possibility of developing melanoma against the background of intradermal MN, as well as due to the difficulty of clinically distinguishing borderline and mixed MN from dysplastic nevus, in order to avoid malignancy in ordinary MN, they should not be subjected to constant friction with clothing, contact with irritating substances, and mechanical hair removal from them is unacceptable. surface /25/.
Melanoma-dangerous MNs include congenital and dysplastic nevi. Congenital MN are benign pigmented tumors consisting of nevus melanoblast-derived cells. arising as a result of impaired differentiation of melanoblasts in the period between 10 weeks and 6 months of intrauterine life. They occur in 1% of Caucasian children, are detected at birth or during the first year of a child's life and come in different sizes: from tiny to gigantic. Any of them can develop melanoma. Clinically, they are light or dark brown in color, slightly raised above the skin level and sometimes covered with hair (hair growth does not begin immediately), and have a round or oval shape. Their boundaries are clear or blurred, the shape is regular or irregular, the surface has a preserved skin pattern or is bumpy, wrinkled, folded, lobulated, covered with papillae resembling cerebral convolutions (loss of skin pattern occurs when the reticular layer of the dermis is involved in the pathological process (blue congenital MN), color - light or dark brown. They are localized on any part of the skin and in 5% of cases they are multiple (in this case, one of them is large). Larger nevi have a soft consistency when palpated.
Congenital MNs can be small (up to 1.5 cm), large (up to 20 cm) and giant. Congenital MNs are practically indistinguishable from acquired conventional MNs, the only difference is a diameter of more than 1.5 cm (acquired MNs do not have such a diameter), therefore, it is currently proposed that MNs with a diameter of more than 1.5 cm be regarded as congenital MN or dysplastic nevus /2/. Large and giant congenital MNs, in contrast to small congenital MNs, which are solitary in 95% of cases, are usually represented by large or very large MNs, occupying part or all of the anatomical region (trunk, limb, head and neck), but in combination with many small ones MN (Fig. 3).
Rice. 3. Congenital melanocytic nevus.
In this case, nevus cells form ordered accumulations in the epidermis and dermis in the form of layers, nests or strands. The presence of nevus cells in the lower third of the reticular layer of the dermis or in the subcutaneous tissue indicates the congenital nature of MN /19/ Nevus cells are found, in contrast to acquired MN, also in the appendages of the skin, bundles of nerve fibers, muscles that raise the hair, in the walls of the blood and lymphatics vessels. In large and giant congenital MNs, nevus cells sometimes penetrate muscles, bones, and dura mater.
Unlike acquired MNs, congenital MNs do not disappear spontaneously. The risk of developing melanoma against the background of small congenital nevi is 1-5%, giant ones - 6.3% (and in 50% of cases, melanomas develop at the age of 3-5 years). The prognosis for melanoma growing from a large congenital MN is always unfavorable, since it is usually detected in the later stages of development.
Dysplastic nevus (DN) (syn.: Clark's nevus, atypical nevus) is an acquired pigmented neoplasm, characterized histologically by random proliferation of atypical melanocytes. It occurs in 5% of the population /8/ (including 30-50% of patients with sporadic and all patients with familial melanoma) and occurs on clinically unaffected skin or against the background of complex or (rarely) borderline MN. DNs appear later than acquired MNs—shortly before the onset of puberty or throughout life until old age. Their development is promoted by insolation. They are not characterized by spontaneous involution. DN can be sporadic (30-50% of cases) or hereditary, transmitted in an autosomal dominant manner (DN syndrome or familial atypical MN syndrome). DN syndrome and familial melanoma are caused by mutations of various genes, most often localized in chromosome segments 1p36 and 9p21 /19/. Clones of mutant melanocytes can be activated under the influence of photons from sunlight.
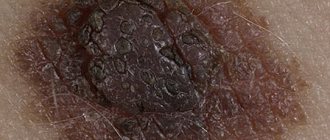
DN occupies an intermediate position between acquired MN and superficially spreading melanoma /2/ and is clinically manifested as: a spot with individual areas raised above the skin level (papule against the background of the spot), large (more than 15 mm in diameter) in size, uneven (motley, reminiscent of scrambled eggs - fried egg or target) coloring, asymmetry, irregular borders (the edges are partly fuzzy, uneven) (Fig. 4).
Rice. 4. Dysplastic nevus
Located mainly on the torso and limbs. Transformation of DN into superficial spreading melanoma occurs in 18-35% of cases /2.9/. The risk of developing melanoma in DN in persons with immunosuppression (organ transplant recipients, etc.) increases significantly, and in DN syndrome transformation into melanoma occurs in 100% of cases. It is estimated that in the presence of one DN, the likelihood of developing melanoma increases by 2 times, compared with cases where it is absent, and in the presence of 10 or more - by 12 times /2/. The risk of malignant transformation is especially high if a relative has more than 100 elements of DN or melanoma.
Histologically, DN is characterized by: hyperplasia and proliferation of melanocytes, which in the form of spindle-shaped cells are located in a single row along the basal layer of the epidermis (lentiginous melanocytic dysplasia) or in the form of epithelioid cells form scattered nests of irregular shape (epithelioid cell melanocytic dysplasia); atypical melanocytes (large cell size, polymorphism of cells and their nuclei, nuclear hyperchromasia); Nests of melanocytes are also characteristic: scattered, irregular in shape, forming “bridges” between the interpapillary processes of the epidermis; spindle-shaped melanocytes are oriented parallel to the skin surface; there is a proliferation of collagen fibers in the dermal papillae and fibrosis (a variable sign) / 19 /.
In connection with the problem of melanoma formation in melanoma-dangerous MN, it is important to take into account that its cytological diagnosis is not sufficiently reliable, therefore, for the purpose of diagnosis and differential diagnosis, a diagnostic biopsy of the neoplasm is performed.
Excisional biopsy for the purpose of histological examination, a reliable method for detecting melanoma, is safe and recommended for MNs less than 1.5 cm in diameter and carried out 2 mm from its edge /4.12/.
An incisional (partial) biopsy is performed by an oncologist for very large (congenital) MNs /4/. In particular, with the sudden appearance of longitudinal melanonychia, to exclude acral-lentiginous melanoma or Bowen's disease of the nail matrix (also causing longitudinal melanonychia), a biopsy is performed with a 3-4 mm punch (through the nail plate and matrix to the phalangeal bone) /26/.
Superficial biopsy (“cutting”, curettage, etc.) is unacceptable, because does not make it possible to determine the depth of tumor invasion /19/.
Differential diagnosis of MN with various dermatoses and skin neoplasms is presented in Table 1.
Table 1.
To the differential diagnosis of melanocytic nevus
| Form MN | Dermatosis/skin tumor |
| Border | Freckles, lentigo simplex, lentigo solar (senile), café au lait spots, congenital MN, macular nevus, xeroderma pigmentosum, dysplastic nevus, Dubreuil's melanosis. |
| Mixed | Seborrheic keratosis, Kaposi's sarcoma |
| Intradermal | Dermatofibroma, wart vulgaris, trichoepithelioma, juvenile xanthoma, syringoma, molluscum contagiosum, accessory nipple, pyogenic granuloma, neurofibroma, acrochordon, cystic basal cell carcinoma |
| Congenital | Dysplastic nevus, blue nevus, Becker's nevus, verrucous epidermal nevus, café au lait spots |
| Dysplastic nevus | Congenital MN, Dubreuil's melanosis, Spitz nevus, pigmented basal cell carcinoma |
The differential diagnosis of MN with Dubreuil's precancerous limited melanosis and some forms of melanoma should be discussed in more detail.
Precancerous melanosis limited by Dubreuil (syn.: Hutchinson's melanotic freckle), in contrast to intradermal MN, has a larger (over 20 mm) diameter, irregular outline, uneven pigmentation; it occurs on exposed areas of the skin (usually on the cheeks in older people) and is characterized by slow progression to melanoma; Histological examination reveals the structure of melanoma in situ.
Acral-lentiginous melanoma, in contrast to intradermal MN, is characterized by a brown or black plaque with unclear contours and uneven coloring /2/.
Desmoplastic (amelanotic) melanoma, in contrast to intradermal MN, looks like a non-pigmented spot or papule, reminiscent of a scar or scar, and in the “vertical growth” phase it is characterized by a dense node, most often developing in the head and neck area in people of the 6th-7th decade life, may occur in association with acral-lentiginous melanoma or de novo /14/; microscopically consists of spindle-shaped cells located between thin layers of collagen, which are often formed into bundles.
Differential diagnosis of intradermal MN with superficial spreading and nodular forms of melanoma is carried out according to the “FIGARO” rule:
F - shape. Melanoma is characterized by a convex shape (which is best seen in side lighting). Melanoma in situ and acral lentiginous melanoma are flat.
And - change in size. Accelerated growth is one of the most important signs of melanoma.
G - the boundaries are incorrect. The tumor has “ragged” edges.
A- asymmetry - one half of the tumor is not similar to the other.
P - large sizes (usually more than 6 cm)
O- the color is uneven - randomly scattered brown, black, gray, pink and white areas /9/.
Dark brown and black MNs in people with fair skin color should be considered the most suspicious for melanoma. You should also be suspicious of MN with bluish, reddish and white areas on the surface. However, changes in the color of MN may be due to factors not related to its malignant transformation: pregnancy, puberty, taking glucocorticoid hormones, exposure to external factors, including solar radiation. In such cases, all MNs or MNs of the same localization that were affected by external factors change simultaneously. Only changes in a single MN require oncological alertness.
When collecting anamnesis, the dermatologist must exclude other causes of sudden changes in MN that are not related to its transformation into melanoma. Thus, a sudden change in color, surface or size in the presence of pain, itching, ulceration and bleeding can be caused by the formation of a cystic enlargement of the hair follicle, an epidermal cyst in the MN, the development of folliculitis in it, as well as trauma, hemorrhage, compression or thrombosis of skin vessels. With such changes, dynamic observation is required with serial photography of the elements until the effects of injury or inflammation pass (usually 7-10 days), and in some cases a histological examination is required.
Among the instrumental methods for excluding melanoma, epiluminescence microscopy is currently used - a non-invasive method for studying skin formations in a special immersion environment using a dermatoscope, as well as a computer diagnostic method in which images recorded using a digital video camera are stored in computer memory and compared with the existing one based on certain characteristics. database /1/.
The accuracy of histological diagnosis of melanogenic skin tumors increases when using the “diagnostic ploidometry” method /10/.
Treatment tactics
Although in the vast majority of cases acquired MN do not require treatment, it is still undertaken in some conditions.
Indications for excision of conventional MNs may include:
- the patient’s desire to remove it for cosmetic reasons, however, it should be taken into account that histological preparations of “disfiguring MN” often reveal atypical cells /25/;
- location in places difficult for self-control (scalp, perineum, etc.), this primarily applies to hyperpigmented MN and if there is a personal or family history of DN;
— presence of signs of atypia in the MN: uneven distribution of pigment, jagged and unclear boundaries, relatively large size (more than 5 mm);
- atypical evolution of MN, including a sudden change in size and shape /13/;
— MN with a high risk of malignancy (lentigo maligna, giant congenital MN); DN, including as part of spotted MN; prophylactic removal prevents the possibility of melanoma even with a significant number of MNs /25/;
- although the features of the anatomical location are not considered as an indication for removal of MNs, nevertheless, intensely pigmented MNs of acral localization in the extremities, as well as on the mucous membrane, should be removed, as well as MNs of the subungual region and conjunctiva, since the possibility of DN of such localization should cause caution regarding its transformation into melanoma /22/.
If the element is frequently repeatedly irritated, it is better to remove it than to miss melanoma or other malignant tumor /11/; at the same time, MNs located under a belt, bra, or collar do not have to be removed if they look benign /25/;
Based on this, the MN can be surgically removed in case of: rapid change in the element, atypical clinical picture, suspicious for melanoma, for cosmetic reasons, repeated injury to the element /13/.
The indication for immediate excision of the MN is the presence of at least one of 7 signs of its sudden (within one or several months) change:
- increasing the area and height of the element;
- increasing the intensity of pigmentation, especially if it is uneven;
- signs of local regression;
- the appearance of a pigment corolla around the MN, the appearance of satellite elements;
- inflammatory reaction in the MN;
- itching;
- erosion and bleeding.
Removal of MN must be complete and performed surgically with mandatory histological examination. After partial removal, the MN repigments and recurs, forming pseudomelanoma /23/. Other removal methods (electrocoagulation, cryodestruction, dermabrasion, laser) for pigmented formations of the skin and mucous membranes should not be performed, because do not provide documentary verification of the diagnosis /12/.
When starting treatment for MN, it should be taken into account that with its non-radical removal, the cosmetic outcome is often unpredictable, because treatment may lead to relapse with less favorable consequences than before treatment /25/.
All small congenital MNs that look unusual (uneven coloring, irregular outline, etc.) are subject to surgical removal before the patient reaches the age of 12 years. Giant congenital MN is removed as early as possible. Full-thickness skin flaps are used to close the defect. For large sizes, they resort to expander plastic or plastic with local tissues.
Treatment of DN should be carried out by an oncologist.
Prevention of melanoma consists of early and active detection of pre-melanoma lesions (primarily DN and lentigo maligna), the need to allocate patients with their presence to a “risk group” with constant dynamic monitoring of macroscopic changes in these spots.
Patients with DN should be informed about the signs of transformation of these MNs into melanoma and independently regularly monitor the nature of individual elements. They are advised to avoid exposure to the sun and use sunscreen (Anthelios XL60+) when going outside.
V.A. Molochkov
Moscow Regional Research Clinical Institute named after M.F. Vladimirsky)
Molochkov Vladimir Alekseevich - Doctor of Medical Sciences, Professor, Head of the Clinic of Dermatovenereology and Dermato-Oncology
Literature:
1. Demidov L.V., Kharkevich G.Yu. Markina I.T. and others. Melanoma and other malignant neoplasms of the skin/Encyclopedia of Clinical Oncology. Guide for practitioners / M.I. Davydov et al. - M.: RLS-2005.-P.341-364;
2. Borisova G.N., Kudryavtseva G.T. //Vestn. dermatol.-2006.-No.3.-P.43-45;
3. Dermato-oncology /Ed. G.A. Galil-ogly and others - Medicine for all - 2005;
4. Makin I.L.. Pshenistov K.P. Selected issues of plastic surgery-1999.-No. 1-Yaroslavl-DIA-press;
5. Molochkov V.A. //Aesthetic Medicine-2005.-No. 3-P.266-270;
6. Molochkov V.A. //Russian Journal of Skin and Venereal Diseases-1998.-No.2.-P.68-76;
7. Organizational technology of interaction between dermatovenerological and oncological services to provide specialized care to patients with pre-tumor and malignant skin pathologies - Guidelines No. 2003/60-M, 2003;
8. Paltsev M.A., Potekaev N.N., Kazantseva I.A. and others. Clinical and morphological diagnosis of skin diseases (atlas) - M.: Medicine-2004;
9. Fitzpatrick T., Elling D.L. Secrets of dermatology /Trans. from English - M.S.Pb - BINOM - Nevsky dialect - 1999;
10. Chervonnaya L.V. Diagnosis of skin tumors of melanocytic origin // Abstract. dis. .. doc. medical sciences-2003;.
11. Chissov V.I., Romanova O.A., Moiseev G.F. Early diagnosis of melanoma. - M.: Yulana Trade, 1998;
12. Anderson RG //Select. Read. Plast. Surg.-1992.-Vol.7.-P.1-35;
13. Barnhill RL, Lewellin K. Benigh Melanocytic Neoplasm /In: Dermatology /Ed. J.Bolognia et al.-Mosby-Edinburg-2003.-P.1757-1787;
14. Barnbill RL, Mihm MC Histopathology and precursor lesions /In: Cutaneous melanoma, 3ed/Ed. CM Balch et al.-St.Louise, Quality Medical.-1998.-P.103-133;
15. Bhawan J.//Cutan Pathol.-1979.-Vol.6.-P.153;
16. Bogdan I., Smolle J., Kerl H. et al.//Melanoma Res.-2003.-Vol.13.-P.213-217:
17. Clemente C., Zurrida S., Bartoli D. et al. //Hitopathology-1998.-Vol.27.-P.549-555;
18. Crulich AE et al.//Int.J.Cancer-1996.-Vol.67.-P.485;
19. Elder DE, Elenitsas R., Murphy GF, Xu X. Benign pigmented lesions and malignant melanoma / Lever's Histopathology of the Skin .Ed.: DEElder-9th ed- Lippincott Williams & Wilkins-Philadelphia-2005.-P.715-803 ;
20. Eskandrapour M., Hashemi J., Kanter L. et al. Frequency of UV-inducible NRAS mutations in melanomas of patients with germline CDKN2A mutations //J.Natl.Cancer Inst.-2003.-Vol.95.-P.790-798;
21. Goettman-Bonvallot S., Andre J., Belaich S. // J.Am.Acad. Dermatol.-1999.-Vol.41.-P.17-22;
22. Kopf AW, Waldo E.//Aust.J.Dermaatol.-1980.-Vol.21.-P.59;
23. Kornberg R., Ackerman AB//Arch.Dernatol.-1975.-Vol.111.-P.1588;
24. Maize JC, Foster G. //Clin. Exp. Dermatol. - 1979. - Vol.4. - P.49;
25. Rhodes AR Benign neoplasias and hyperplasias of melanocytes //Fitzpatrick's dermatology in general medicine - 5th ed.//Ed. IMFreedberg et al. —Mc Graw-Hill-New York. - 1999. - P.1018-1059;
26. Rich P. //J.Dermatol.Surg.Oncol.-1992.-Vol.18.-P.673-682;
27. Rock B., Hood AF, Rock JA // J.Am.Acad. Dermatol.-1990.-Vol.22.-P.104-106;
28. Scher RK, Silvers DN // J.Am.Acad. Dermatol.-1991.-Vol.24. -P.1035-1036;
29. Shelly WB //Arch. Dermatol.-1960.-Vol.81.-P.208;
30. Tajima Y., Nakaijama T., Sagano I. et al //Am.J.Dermatopathol-1994.-Vol.16.-P.301-306.