The inflammatory process on the skin, especially on the face, is a great stress for the body. Various pimples and pustules bring a lot of inconvenience to a person. But their reasons can be completely different. Some are less dangerous, others can lead to serious consequences. Accordingly, they all require a different treatment approach. Let's look at how to distinguish a boil from a pimple by location, appearance, pain, ripening time and other manifestations, and try to understand the reasons for their appearance.
What is a boil?
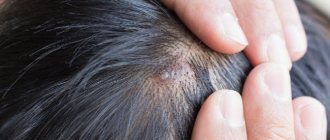
A boil develops when a hair follicle becomes inflamed.
Photo: Mahdouch at French Wikipedia (Creative Commons Attribution 1.0 Generic license) Research shows that skin diseases are one of the leading reasons for visits to primary health care. A striking example of a disease in this group is the occurrence of boils, which are purulent-necrotic inflammations of hair follicles and adjacent tissues, including the sebaceous glands. They most often occur in adolescence and early adulthood1.
Localization of boils
In most cases, boils occur in areas exposed to pollution and/or mechanical stress - on the hands, forearms, back of the neck, buttocks, lower back, thighs. In rare cases, ulcers appear in unexpected places - in the ear canal, on the outer and inner surfaces of the nose, labia, etc. However, boils never form on areas of the skin that are devoid of hair - the palms and palmar surfaces of the fingers, soles.
What is the difference between a boil and a carbuncle?
A carbuncle is a purulent-necrotic inflammation of several hair follicles at once, merging into one purulent focus (Fig. 1). Often it is a complication of a boil. Carbuncle occurs much less frequently than furuncle, and the main group of patients consists of middle-aged and elderly people.
Figure 1. How a boil differs from a carbuncle. Source: IQWiG/NCBI
1.General information
A furuncle, or, in common parlance, a boil, is an acute inflammation in a local sealed volume, accompanied by intense suppuration and necrosis of the affected tissue.
The furuncle of the external auditory canal, thus, is an abscessing purulent-inflammatory process that affects the hair follicles or sebaceous glands, which abound in this part of the hearing organs. In the specialized literature, the synonymous name “acute limited external otitis” is also used; In the International Classification of Diseases, the nosological unit “abscess of the external ear” is recorded. Purulent melting and necrotization extends not only to the surface layer of the skin, but also to the subcutaneous tissue, leaving a scar defect when resolved.
Like other pyoderma (purulent inflammation of the skin), a boil of the external auditory canal sharply reduces the quality of life, bringing a lot of painful and uncomfortable sensations. In addition, the location and anatomical features of the external auditory canal pose a very real risk of complications, including severe and even fatal ones.
A must read! Help with treatment and hospitalization!
Causes
A boil develops as a result of infection of the hair follicle by pathogenic bacteria, often in combination with a decrease in local and systemic immunity. In the vast majority of cases, the cause of inflammation is Staphylococcus aureus, less often Staphylococcus pyogenes albus.
One of the important triggering factors in this case is the disruption of the normal composition of the skin microflora, due to which pathogenic staphylococci are able to remain on its surface for a long time. This is primarily due to non-compliance with personal hygiene rules.
Risk factors
Violation of the composition of the skin microflora contributes to the deterioration of the immune system, which can be caused by the following pathologies and factors:
- Infectious diseases: AIDS, chronic tuberculosis.
- Chronic somatic pathologies: hepatitis, bronchitis, pyelonephritis.
- Endocrine diseases: diabetes mellitus, endocrine obesity.
- The presence of malignant tumors in the body and their treatment: radiation or chemotherapy.
- Long-term use of glucocorticosteroids.
- Improper, unbalanced nutrition, leading to hypo- and vitamin deficiency.
Local changes in the skin that contribute to the appearance of boils include:
- Hyperhidrosis – increased sweating.
- Frequent skin trauma, scratches and cuts.
- Dermatological pathologies: eczema, acne, psoriasis.
Stages of boil development
When a hair follicle becomes infected, a pustule is first formed containing neutrophils (white blood cells responsible for the immune response), pathogenic staphylococci and fibrin. Next, the bacteria descend down the follicle, provoking inflammation, which leads to the formation of an infiltrate followed by necrosis (death) of the surrounding tissues. At the same time, tissue melts around the affected area, due to which pus is formed and the boil matures. Purulent exudate accumulates under the epidermis, around the mouth of the follicle. Further, together with the necrotic rod and dead hair, it breaks through and comes out. Over time, a scar forms at the site of the ruptured boil.
Based on pathogenesis and clinical features, it is customary to distinguish 3 successive stages of boil development, which take about 7-10 days. These include:
- Infiltration stage. Accompanied by infiltration (leakage of blood elements and products of the inflammatory process) of the tissues around the hair follicle. Takes 3-4 days.
- Stage of suppuration and necrosis. It begins with the formation of a characteristic purulent-necrotic core. Intoxication syndrome also occurs. At the peak of clinical manifestations, the covering of the purulent core is opened, and purulent masses are released from the resulting hole. After this, the symptoms subside.
- Recovery stage. It begins with the formation of granulation tissue in the form of a crust at the site of opening. 3-4 days after this, a connective tissue scar appears, initially having a red-blue color, but gradually turning pale and acquiring a flesh color. The entire stage takes up to 10 days.
Publications in the media
Furuncle - acute purulent-necrotic inflammation of the hair follicle and surrounding soft tissues •
Furunculosis is multiple lesions with boils that appear simultaneously or sequentially one after another in different parts of the body. Most often, boils are localized in areas of the skin exposed to contamination (forearms, back of the hand) and friction (back of the neck, lower back, gluteal region, thighs).
Etiology . Golden, less often white staphylococcus.
Risk factors • Skin contamination and microtraumas • General exhaustion • Chronic diseases • Vitamin deficiencies • Diabetes.
Pathomorphology • Stage of serous infiltrate - cone-shaped infiltrate with regional hyperemia up to 1-1.5 cm in diameter • Purulent-necrotic stage - appearance of a purulent pustule at the apex • Stage of rejection of the necrotic core and healing.
Clinical picture
• During the formation of a pustule in the form of a nodule - slight itching and tingling • On days 1–2, an inflammatory infiltrate appears, protruding cone-shaped above the level of the skin, which turns red and becomes painful when touched • At the top of the infiltrate, a small accumulation of pus with a black dot appears (necrosis) in the center • The pustule usually breaks through and dries up, and on days 3–7 the infiltrate purulently melts and the necrotic tissue in the form of a rod, together with the remains of the hair, is excreted with pus • The resulting wound is cleaned, filled with granulation tissue and heals. The swelling around it gradually decreases, the pain disappears. A small, whitish, somewhat retracted scar remains at the site of inflammation.
• When the boil is localized in the external auditory canal, severe pain occurs in the nose • In the facial area (lips, forehead), as well as on the scrotum, boils are accompanied by significant swelling of the surrounding tissues
• A severe clinical course is typical for boils of the upper lip, nasolabial fold, nose, and periorbital region. Thrombophlebitis of the veins with a facial boil can spread through anastomoses to the venous sinuses of the dura mater, which leads to their thrombosis, creating a threat of the development of purulent basal meningitis. Facial swelling quickly increases, dense, painful veins are palpated, the patient’s general condition sharply worsens, body temperature reaches high values (40–41 °C), neck rigidity and blurred vision may be expressed.
Laboratory research . Leukocytosis with a shift in the leukocyte formula to the left, an increase in ESR.
TREATMENT
Management tactics • Patients with severe systemic inflammatory response syndrome, when boils are localized in the nasolabial triangle, and in the presence of severe concomitant diseases (DM, tumors) are subject to hospitalization.
Conservative treatment • Thorough cleansing of the skin around the source of inflammation •• 70% ethyl alcohol •• 2% salicylic alcohol •• 0.5–1% alcohol solution of brilliant green •• In the formative stage - 5% alcohol solution of iodine • Antibacterial therapy, first empirical, and then taking into account the data of bacteriological research •• oxacillin •• cefazolin • NSAIDs • Physiotherapeutic treatment: UHF, ultraviolet radiation • Detoxification therapy, immunomodulators (if necessary).
Surgery . _ Opening the boil with removal of the necrotic core.
Complications • Lymphangiitis • Regional lymphadenitis • Carbuncle • Acute thrombophlebitis • Sepsis, often develops with facial boils, due to attempts to squeeze out the contents, cutting it off while shaving.
Prevention • Compliance with personal hygiene requirements • Preventing clothing from rubbing areas of the skin where a boil may form.
Course and prognosis • With timely and correct treatment, the prognosis is favorable • In exhausted, weakened patients, if complications occur, the prognosis is serious.
ICD-10 • L02 Skin abscess, boil and carbuncle
Is a boil dangerous? Possible complications
In most cases, with timely treatment, boils do not pose a serious danger. But when trying to independently squeeze out a purulent-necrotic rod, inadequate local therapy, or the addition of a secondary infection, dangerous complications can develop.
Local complications include purulent lesions of the skin and subcutaneous tissue: furunculosis, carbuncles, abscesses and phlegmon. Damage to adjacent blood vessels and lymph nodes in the form of phlebitis, thrombophlebitis, and lymphadenitis is also possible.
The greatest danger is represented by boils located in the area of the nasolabial triangle and higher on the face and ear canal, since there is a high risk of spread of purulent masses and pathogenic bacteria into the cranial cavity through blood vessels. This can lead to damage to the meninges (meningitis, arachnoiditis) and directly to the brain tissue (encephalitis, brain abscesses). In rare cases, a boil can cause purulent masses and bacteria to enter the systemic circulation with the development of sepsis.
Important! A burst boil that is not treated properly poses a particular danger to the patient and others. An ruptured boil can cause infection of other follicles with the formation of furunculosis, as well as an entry point for secondary infections. In addition, the released purulent masses can become a source of infection for other people who come into contact with it directly or indirectly (through household items).
Treatment of furunculosis.
In order to cope with the disease, be sure to contact a specialist and follow all his instructions.
During the treatment of furunculosis, the patient will have to limit water procedures or even completely abandon them. The exception is extensive furunculosis: in this case, warm baths with potassium permanganate are recommended to disinfect the skin. Instead of washing and taking a bath, visiting a bathhouse, or taking a shower, you will need to wipe healthy skin with non-aggressive antiseptic solutions, for example, salicylic alcohol or furatsilin solution.
Personal hygiene during the treatment of furunculosis is extremely important - it was already mentioned above that microtraumas of the skin can lead to the further development of this disease. Therefore, it is necessary to frequently change underwear and bed linen, and treat any, even the smallest, cuts and scratches with a solution of brilliant green.
At the stage of boils maturation, the skin around them must be treated with antiseptics.
Antibiotics for furunculosis are also used as prescribed by the attending physician - in cases of abscesses and in the chronic course of the disease. If general diseases are diagnosed, the patient is exhausted, or has a decreased immune status, a specialist may prescribe antibiotics in the form of intramuscular injections.
To prevent complications such as cellulitis or abscess, experts recommend electrophoresis in combination with antimicrobial drugs.
If an abscess develops as a result of the disease, then the boil is opened under local anesthesia, and the purulent-necrotic masses are removed.
Prescription of general strengthening drugs and vitamins.
Regardless of the stage of furunculosis, it is necessary to correct the concomitant pathology: sanitize chronic infectious foci, treat diseases of the gastrointestinal tract, endocrine disorders, and so on.
During treatment, it is necessary to exclude spicy and fatty foods from the diet, and eat more food rich in vitamins and protein, which promote tissue regeneration. Products with a high fiber content promote good gastric emptying, which helps avoid dysbiosis, and this is very important for furunculosis. Instead of tea and coffee, it is better to drink rosehip infusion, compote or fruit drink.
Symptoms of a boil
In most cases, boils occur with fairly characteristic symptoms, which vary depending on the stage of development. In general, patients may have the following complaints:
- General weakness, increased body temperature up to 38°C, headache.
- Tingling, itching in the area where the boil forms, which after a few days is replaced by sharp pain.
- Redness and thickening of the skin in the area of inflammation, which protrudes cone-shaped above the skin.
- The formation of a small whitish purulent head in the center of the compaction, which opens after a few days.
- Discharge of yellowish purulent contents from the hole formed after opening the pustule. At the same time, pain is significantly relieved and the general condition of a person improves.
- Manifestations of furunculosis can vary depending on the location and are accompanied by uncharacteristic features. For example, when a purulent focus forms in the area of the upper lip or eyelids, pronounced swelling is observed, and when a boil occurs in the area of the auditory canal, a severe headache spreading to the lower jaw, as well as hearing impairment, come to the fore.
Symptoms
The boil develops gradually, going through three stages: formation of infiltrate, suppuration and rejection of the purulent core, healing. At the first stage, tingling, burning, and pulsation are felt. The area gradually turns red, becomes denser and slightly rises above the skin.
In the center of the cone-shaped inflamed area, the upper part of the purulent capsule, the pustule, is visible. On the fourth day, the abscess acquires its maximum size - from one to three cm in diameter. After “ripening,” the pustule opens (usually spontaneously or from an accidental touch), and pus comes to the surface. The capsule is separated by light pressure on adjacent areas of the skin or “pushed out” with special preparations.
If boils appear in several places or after the healing of one abscess the next one quickly forms, then it is necessary to carry out a comprehensive diagnosis to identify the cause of the disease.
When to see a doctor?
In most cases, a person can independently cope with one, uncomplicated boil. However, it is recommended to seek medical help if there is a significant disturbance in the general condition or the first signs of complications.
Alarming symptoms and changes that indicate the need to contact specialists are:
- Simultaneous appearance of more than 1 boil.
- The appearance of a boil on the face.
- Rapid deterioration in health.
- Severe pain in the area of the boil, increased body temperature to 39°C or more.
- Lack of positive dynamics, despite the treatment.
- Persistence of the inflammatory process for more than 2 weeks.
- Constant recurrence of boils.
How to treat a boil so as not to harm your body?
The most correct recommendation would be to consult a doctor - surgeon or dermatologist, do not self-medicate . The doctor will make a diagnosis and prescribe the necessary treatment - conservative or surgical.
Conservative treatment is possible only at the first stage of the disease.
The main method of treating a boil is surgical . Only timely opening of the abscess, ensuring the outflow of purulent contents, followed by drainage of the wound will lead to success.
The opening and drainage of the boil in our clinic is performed under local anesthesia (lidocaine, ultracaine, novocaine) and for the patient this procedure is painless and is performed on an outpatient basis.
Qualified surgeons at ACMD-MEDOX will help you cope with surgical troubles. Contact us, we will be happy to help!
Diagnostics
The diagnosis of “boil” is usually established on the basis of characteristic clinical changes. However, in order to monitor the patient’s general condition, early detection and prevention of complications, the following laboratory and instrumental diagnostic methods can be used:
- General blood and urine tests (CBC, UAM).
- Biochemical blood test with determination of glucose levels.
- Blood test for HIV using enzyme-linked immunosorbent assay (ELISA).
- Determination of hepatitis B and C virus markers by ELISA.
- Bacterial culture of a sample of purulent masses to identify the pathogen and its sensitivity to main antibiotics.
For recurrent and multiple boils, fluorography or radiography of the chest organs, ultrasound examination of the abdominal organs and kidneys, etc. can be additionally performed.
Differential diagnosis of a boil is carried out with other dermatological and infectious diseases, which may be accompanied by similar symptoms, including:
- Hidradenitis suppurativa,
- Erythema nodosum,
- Anthrax,
- Lupus,
- Actinomycosis.
3. Symptoms and diagnosis
The furuncle of the external auditory canal in terms of dynamics does not differ from abscess processes of other localization: the infiltration stage is followed by violent suppuration, then the abscess opens (spontaneously or during medical intervention - but in no case should this be done independently!), and after passive or forced evacuation of purulent-necrotic masses results in fairly rapid healing and scarring. At the stage of infiltration, pain is expressed; the pain can be very severe, throbbing or shooting in nature. As a rule, body temperature is elevated, sometimes to high values. Any mechanical impact, including chewing, swallowing or talking, sharply increases pain. Severe swelling and a significant size of the boil can lead to significant obstruction of the ear canal and, accordingly, to transient hearing loss on the affected side. When the peripheral endings of the vagus nerve are involved in the process, coughing and vomiting are possible.
The diagnosis usually does not cause any difficulties for an experienced otolaryngologist. In case of repeated or multiple boils, measures are taken to laboratory identification of the infectious agent; as necessary, an endocrinologist, infectious disease specialist and other specialized specialists are involved in the diagnostic and treatment process.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of a boil
The boil, in the vast majority of cases, is subject to local treatment, which depends on the stage of its development. The purpose of the therapy is to prevent complications, cleanse the purulent focus and prevent the formation of rough scars.
Drug treatment
At the infiltration stage, ichthyol dressings, warming with dry heat and UHF therapy can be used. After opening, bandages with hypertonic sodium chloride solution, turunda with chloramphenicol and methyluracil are indicated.
To reduce body temperature and suppress pain, non-steroidal anti-inflammatory drugs (NSAIDs) can be used: ibuprofen, paracetamol. Depending on the accompanying changes, vitamin complexes, antihistamines, immunomodulators, etc. are used. If complications are suspected, antibacterial drugs can also be prescribed.
Local treatment with ointments
Local remedies are often used to combat boils.
Photo: Genrix20061.mail.ru / Depositphotos Local therapy using various ointments plays an important role in treatment. Considering the large number of topical medications on the market and the stage of the disease, it is better to consult a doctor before choosing a drug, especially if a boil has developed in a child.
At the infiltration stage, it is recommended to use antiseptic ointments with a so-called pulling effect: ichthyol, heparin, synthomycin.
When opening a boil on your own, treatment of the resulting skin defect with antibacterial soap is indicated, after which it is necessary to apply an antiseptic. In order to prevent local purulent complications, bandages with agents that have a local antibacterial effect (levomekol or tetracycline ointment) are used. It is recommended to change the dressing 2-3 times a day until healing, washing the wound with warm water and soap.
Surgery
In some cases, with severe pain or the risk of complications, a decision is made to open the boil. To do this, a small incision is made above the pustule, through which purulent-necrotic masses are removed. After surgery, the affected area is treated with antiseptic solutions, and less commonly, systemic antibiotics are prescribed.
Tips for treatment at home
Small, single boils can be treated at home. To speed up the recovery process and prevent the spread of infection into adjacent tissues and blood vessels, the following recommendations should be followed:
- Use warm compresses. Resorting to warm compresses several times a day for about 10 minutes will help the boil open and quickly release purulent-necrotic masses.
- Minimize mechanical impact on the boil. You should not try to squeeze out or puncture the boil yourself. This can lead to a breakthrough of the purulent-necrotic core into deeper tissues.
- Observe hygiene rules. After handling an opened boil and coming into contact with its discharge, you must wash your hands thoroughly. It is also important to use disposable materials for compresses and bandages and to wash clothing and fabrics that have come into contact with the contents of the boil.
Traditional treatment
Various folk recipes can be used as auxiliary therapy. However, it is important to note that in the absence of positive dynamics and the first signs of worsening local changes or general condition, you must immediately seek qualified medical help.
Some of the most popular folk recipes are:
- Honey cake. To prepare, mix one tablespoon of honey and the same amount of wheat flour. Next, it is applied to the boil until the pustule is opened. It is believed that it helps the purulent focus to clear faster and better.
- Aloe or Kalanchoe. A freshly cut aloe or Kalanchoe leaf is applied with the cut to the skin for several hours to the area of infiltration. This method is suitable for the initial stages of disease development.
- Potato. Peeled, washed potatoes are cut into slices and applied to the boil. This bandage should be changed 3-4 times a day.
To make the boil go away faster, you can use aloe juice. Photo: piyaphunjun.gmail.com / Depositphotos
Furuncle or pimple?
Furuncle or pimple?
A strange formation appeared on the tip of my nose, like a large pimple. It hurts a lot when I touch it. I heard that such pimples are called boils and they definitely need to be removed. Is it so?
T.S. GLEBOVA, Nizhny Novgorod.
Otorhinolaryngologist, doctor of the highest category, candidate of medical sciences Petr Aleksandrovich KOCHETKOV (Moscow) explains.
— As you know, there are hairs on human skin. Each hair has a hair follicle - a follicle. Small hairs grow in people's noses, protecting the sinuses from dust, cold and other irritants.
A furuncle (an inflammatory process of the skin of the nose) occurs due to the penetration of infection into the hair follicle. When bacteria multiply, a purulent focus is formed, which, increasing, rises above the surface of the skin - this is how a boil appears. It can form both in the vestibule of the nose and on its back or wings.
The onset of the disease is acute . There is slight discomfort in the area of the vestibule of the nose, which gradually increases and turns into pain. Pain is often absent at rest and appears when touching the nose, sharp inhalation or exhalation. Upon visual examination, you can notice swelling in the vestibule of the nose, the skin acquires a reddish tint (inflammatory hyperemia).
This condition lasts from several hours to 2-3 days, after which an area of pus breakthrough becomes noticeable at the top of the pimple. However, with boils, purulent discharge can break out not only outside, but also into the tissue. In this case, swelling and soreness of the cheek, upper lip and even eyelids appear. The listed symptoms are an absolute indication for an autopsy of the boil in a specialized ENT office.
There can be many reasons for the development of the disease . The main ones are the following:
- introduction of infection into soft tissues by contact - through dirty hands, hygiene items, poor-quality water;
- the presence of chronic foci of infection, such as adenoids, adenoiditis, sinusitis;
— decrease in the body’s immune forces (immunodeficiency states lead to a reduction in the activity of protective substances on the surface of the skin);
— parasitosis (giardiasis, enterobiasis, opisthorchiasis cause allergies and reduce immunity).
Why are boils dangerous? It would seem that ordinary acne, which can periodically appear on different parts of the skin, should not cause concern. Squeezed out - and order. However, not all so simple.
Firstly, we must not forget that a boil is a purulent-inflammatory process in the soft tissues of the head.
Secondly, there is a peculiarity of the blood supply to soft tissues. The fact is that in the human body, blood from the entire body is directed through the veins to the heart. The blood supply in the head proceeds according to a different pattern: here the blood rushes into the cavity of the skull. This means that an infection in the tissues of the facial skin can travel through the veins to the brain.
What to do if you find a boil? First of all, do not try to open it yourself. The best option is to consult an ENT doctor.
Opening a boil is usually performed under local anesthesia and is painless for the patient. In young children, it is advisable to perform a mini-operation under general anesthesia, since after it it is necessary to do dressings for several days. If the child negatively perceives the autopsy procedure itself, then it will be more difficult to persuade him to bandage it.
The purpose of treating a boil is to drain the pus and ensure constant drainage from the wound. The simplest treatment is a 10% hypertonic sodium chloride solution, a bandage with which is applied to the area of the boil after opening.
Prognosis and prevention
As a rule, recovery occurs 1-2 weeks after the first symptoms appear. Sometimes a small connective tissue scar appears as a residual phenomenon, which gradually acquires a flesh color and becomes hardly noticeable.
It is not always possible to prevent the development of boils, especially when the immune system is weakened. However, the following recommendations can help avoid the development of the disease:
- Maintain good personal hygiene, including regular hand washing with soap and water or using alcohol-based hand rubs. This will reduce the likelihood of disruption of the normal microflora of the skin and infection by pathogenic bacteria.
- Proper treatment of skin damage. The skin around cuts and abrasions should be treated with antiseptics, and the injuries themselves should be bandaged with clean, sterile, dry bandages until they heal.
- Individual use of personal hygiene products. No sharing of towels, sheets, razors, clothing, sports equipment or other personal items is permitted. Due to these items, pathogenic staphylococci are able to be transmitted from person to person.
- Proper, balanced nutrition.
- Complete treatment of concomitant diseases and conditions that can reduce the body's defenses.
Sources
- Shallcross, Laura J et al. “Incidence and recurrence of boils and abscesses within the first year: a cohort study in UK primary care.” The British journal of general practice: the journal of the Royal College of General Practitioners vol. 65.639 (2015).
- Clinical protocol for diagnosis and treatment of “skin abscess, boil and carbuncle of other localizations” Expert Council of the Republican State Enterprise at the Republican Center for Healthcare Development of the Ministry of Health and Social Development of the Republic of Kazakhstan dated December 12, 2014 protocol No. 9.
- Boils and carbuncles. Mayo Clinic.
- Federal clinical guidelines for the management of patients with pyoderma. Russian Society of Dermatovenereologists and Cosmetologists, 2015.