Cutaneous horn is a common dermatological pathology that can occur at any age. But, as medical statistics show, cutaneous horn is rare in children. Older patients are at risk. The cosmetic defect is diagnosed in men and women with equal frequency. The skin abnormality is particularly common in women over 55 years of age. But at its core, the cutaneous horn is a benign neoplasm from the cells of the upper layer of the epithelium.
This disease is called so because of the similarity of the shape of the emerging formation with the horn of an animal. Moreover, the surface of the growth is dense, with keratinized particles as a coating.
Clinical picture
As already mentioned, a new growth appears on the skin, similar in shape to a horn. It has a hard consistency and a rough surface texture. Most often, horny keratoma affects the scalp and neck. Sometimes a cutaneous horn appears on the face. However, these are not the only places of localization. Specialists at the Lasersvit medical center for diagnosing moles are faced with the need to eliminate pathology in various parts of the body. Cutaneous horns are often found on the leg, back, and even on the genitals.
The cylindrical neoplasm has clear boundaries. The color of the growth is dark brown or flesh-colored. The size of the formation varies from a few millimeters to several centimeters. In most patients, keratoma corneum appears in a single copy. But in some patients, our dermatologists diagnosed and removed multiple formations.
As in the diagnosis of other types of tumors, in the case of examining the cutaneous horn, dermatoscopy and histology are used. An integrated approach to making a diagnosis allows you to exclude cancer.
Recognition and treatment of precancerous skin conditions
How to manage patients with solar keratosis? Are “skin horns” a sign of malignancy? Do keratoxanthomas need to be removed and examined histologically?
Most squamous cell carcinomas (SCC) of the skin are preceded by precancerous lesions, the potential for malignancy of which has been established. These precancerous formations include: radiation (solar) keratosis, radiation cheilitis, Bowen's disease, Queyre's erythroplasia, arsenic, tar and post-radiation keratoses and, in our opinion, keratoxanthomas.
Some of these precancerous conditions, such as radiation keratoses, do not show signs of cellular changes for a long time during their natural development. Others, such as Bowen's disease, have microscopic features of intraepidermal carcinoma from the outset. The formation is considered malignant from the moment the basement membrane ruptures or disappears.
Although the most common form of skin cancer is basal cell carcinoma (BCC), it will not be discussed further because it does not have precancerous stages.
Etiology . By the beginning of this century, the carcinogenicity of some chemicals and radiation was established. Soot became the first recognized chemical carcinogen when Percival Potts noted the high incidence of scrotal cancer in young chimney sweeps. In 1906, Hyde [2] reported that ultraviolet (UV) radiation was carcinogenic.
The assumption of a connection between the immune system and some cancers was made by McFarlane Burnett [3], the author of the theory of immune surveillance.
The relationship of the immune system to cutaneous carcinogenesis is well illustrated by the increased incidence of nonmelanoma skin cancers encountered in transplant patients and the relationship between the immunodeficiency observed in HIV-infected patients and various cutaneous malignancies. There remains high interest in the role of papilloma viruses as carcinogens or co-carcinogens for the skin and mucous membranes.
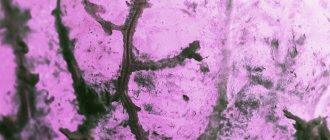
| Figure 1. Radiation keratosis appears in older patients as round, scaly, keratotic, erythematous lesions, typically less than 1 cm in diameter, on sun-exposed skin |
Occasionally, skin cancer can develop at the sites of old scars, fistulas and ulcers.
Radiation keratoses. Clinically, keratoses appear in elderly patients as round, scaly, keratotic, erythematous lesions, usually less than 1 cm in diameter, on sun-exposed skin (Figure 1). The most commonly affected areas are the face, ears, scalp, dorsum of the hands and forearms.
The geographical prevalence of the disease depends on the amount of UV radiation reaching the ground in the area in question, the proportion of the population white-skinned, and the time spent indoors at work and at leisure. In Australia, radiation keratosis is found in 40-50% of people over 40 years of age [4]. The latent period lasts up to ten years. CCs that develop with this keratosis grow slowly and, with the exception of those located on the ears and lips, almost do not metastasize. Malignancy is suspected when the base of the keratosis thickens and there is increased vascularization and inflammation of the dermis.
Histologically, radiation keratosis reveals epithelial dysplasia of varying degrees, which usually also affects the adnexal structures. Superficial damage can be removed by rapid freezing with liquid nitrogen for 10 seconds. Destruction by cauterization or diathermocoagulation, following curettage of horny formations, is no less effective, but more often leaves superficial scars. It is better to excise the indurative zones. Radiotherapy is not used for solar keratoses.
If most of the skin surface is covered with numerous keratoses, the administration of topical 5-fluorouracil may help. It is applied twice a day for two weeks, then take a two-week break and repeat the course again. If severe inflammation develops, strong topical corticosteroids are used.
Preventative measures such as avoiding sun exposure during the heat of the day, wearing a wide-brimmed hat, and using an effective sun shield should be used to both treat and prevent the development of cheilitis.
Radiation cheilitis. This disease is a radial keratosis of the red border of the lower lip. It is caused by exposure to sunlight. Smoking and chronic irritation also contribute to the development of radiation cheilitis. The disease is characterized by the appearance of dry, whitish, gray scaly plaques in which areas of erythema, erosion and ulceration may develop. In the past, whitish areas were called leukoplakia.
PCKs typically develop after a long latent period and behave more aggressively than those developing from ordinary radiation keratosis. As in the case of the latter, with radiation cheilitis, histological changes consist of the appearance of areas of orthokeratosis and parakeratosis with impaired maturation of epidermal cells, increased mitotic activity and various cytological disorders. A good result is achieved by cutting off the damaged area with a razor, capturing the surface layers of the skin. Recently, CO2 lasers have been successfully used.
“Dermal horns.” The “cutaneous horn” can be located in the area of dysplastic or neoplastic epithelium. Horny plugs and growths are sometimes caused by other epithelial changes, such as viral warts, molluscum contagiosum, keratoxanthomas, seborrheic keratosis, or BKC.
Thus, “cutaneous horn” is more likely a clinical marker of pathological changes in the underlying epithelium than a diagnosis itself. Typically, such “horns” are located on parts of the body exposed to the sun, for example on the face and hands (Fig. 2).
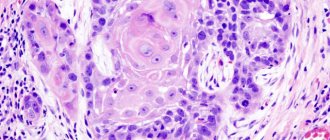
| Figure 2. “Cutaneous horns” indicate areas of dysplastic or neoplastic epidermis |
These formations must be scraped out and sent for histological examination to determine the nature of the changes in the underlying epidermis. If changes similar to radial keratosis are detected, appropriate treatment is carried out. However, if true invasive PCI is detected, tumor excision must be performed.
Bowen's disease. This is the clinical expression of cutaneous PCI in situ [5]. It appears as an asymptomatic, well-circumscribed erythematous scaly patch that expands centrifugally (Fig. 3). There are warty, nodular, eroded and pigmented variants. Manifestations of Bowen's disease can be single or multiple and localized in any area of the skin or mucous membranes.
| Figure 3. Manifestations of Bowen's disease can be single or multiple in any area of the skin or mucous membranes |
Ulceration is usually a sign of invasive growth and may lag intraepithelial changes for years. Invasive PCI develops in 8% of untreated patients.
An invasive tumor has a 13% metastatic potential. The disease must be distinguished from lichen simplex, psoriasis and other papulosquamous dermatoses. In unclear cases, as well as in cases of low effectiveness of local steroids, Bowen's disease should be suspected. The superficial type of BCC is very similar in appearance to Bowen's disease, but, as a rule, it can be distinguished by a slightly raised edge, like a threshold.
Sometimes it is not possible to distinguish these formations from typical flat seborrheic keratosis. In doubtful cases, a biopsy is performed to determine the full thickness of the dysplasia of the epidermis and sometimes the hair follicles and sebaceous glands.
Effective destruction of the epidermis by freezing, cauterization or diathermocoagulation. For best results, cytotoxic agents such as 5-fluorouracil can be applied topically. Relapses are common, mainly due to the carcinoma taking over adnexal structures that were not affected during treatment. If the formation is not too extensive, surgical excision is best.
Erythroplasia of Keir. This disease is PCI in situ of the penis. It appears on the glans of the uncircumcised penis as well-defined, asymptomatic bright red shiny and velvety plaques (Fig. 4). Similar formations can also affect the coronary sulcus or the inner surface of the foreskin.
| Figure 4. Queir's erythroplasia most often develops on the glans penis that has not been circumcised. |
As with Bowen's disease, invasive carcinoma may develop in 10% of cases; it has metastatic potential. Histological changes are the same as with PCI in situ. Treatment consists of circumcision and cryotherapy of the remaining lesions. Of course, careful monitoring of such patients is necessary.
Keratoxanthoma. This is a fast-growing skin tumor that develops in sun-exposed areas (Figure 5). A typical keratoxanthoma is a smooth skin nodule that grows over a few weeks to a size of 10-20 mm with a horny plug in the center. Then growth stops and within three months the formation may reverse.
| Figure 5. Keratoxanthoma is a fast-growing skin tumor that develops in sun-exposed areas. |
In the past, it was unclear whether keratoxanthomas should be considered a benign or precancerous condition; Currently, the opinions of most experts are in favor of the latter. Treatment consists of curettage or wide excision and subsequent histological examination.
Arsenic and tar keratosis. For over a century, inorganic arsenic was used to treat many different conditions until its side effects were discovered. It was gradually replaced by more effective therapeutic agents, resulting in a significant reduction in diseases caused by arsenic.
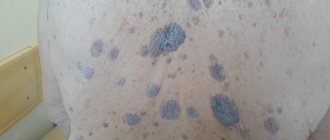
However, high concentrations of arsenic are found in drinking water in some regions of the world, particularly in South America, as well as in naturopathic medicines. More than 40% of affected individuals develop keratosis of the palms and soles (Figure 6). They are more likely to develop multiple skin cancers, including Bowen's disease, BCC, and PCCC [6]. Malignant tumors of internal organs, especially the lungs and genitourinary system, may be detected.
| Figure 6. Arsenic keratoses develop on the palms and soles in more than 40% of cases. |
Skin formations, in the form of small keratotic plaques on the face and hands, are observed in those who work with tar and resin. As a rule, they disappear when contact with these substances ceases, but they can sometimes persist for a long time and become malignant, especially on the scrotum.
| Figure 7. Post-radiation keratosis may develop in the area of a scar caused by radiotherapy or excessive fluoroscopy |
The multiplicity of arsenic and tar keratosis makes radical treatment pointless. In this case, keratolytic powders and rubbing may help. The patient should be periodically examined for malignancy.
Post-radiation keratosis can develop in the area of scar caused by radiotherapy or excessive fluoroscopy. It is found in radiologists, surgeons, dentists and all those who uncontrollably expose their skin to frequent, low-dose X-ray radiation, although the number of such cases is now decreasing.
Histologically, changes in the epidermis are similar to radial keratosis; in the dermis, collagen is actively replaced by scar and hyaline material (Fig. 7).
As in other cases of dysplasia, adequate treatment and careful monitoring of the patient are necessary. References 1. Potter M. Percival Potts' contribution to cancer research. National Cancer Institute 1974; monograph 10: 1-19. Washington Government Printer. 2. Hyde JN On the influence of light in the production of cancer of the skin // Am. j. Med. Sci. 1906; 131: 1-22. 3. Macfarlane Burnett F. Self and Non-self. Cambridge University Press. Cambridge, 1969. 4. Marks R. Non-melanotic skin cancer and solar keratoses: the quiet 20th century epidemic // Int. J. Dermatol. 1987; 26: 201-205. 5. Callen JP Bowen's disease and internal malignant disease // Arch. Dermatol. 1988; 124: 675-676. 6. Graham JH, Helwig EB Bowen's disease and its relationship to systemic cancer // Arch. Dermatol. 1961; 83: 738-758.
Note!
- Radiation keratosis may not appear or change for years. Only a small proportion of solar keratoses develop into invasive PCK, and patients may have multiple skin lesions for years. Malignancy is manifested by induration of the base of the keratosis, increased vascularization and inflammation of the dermis
- It is better to remove superficial formations by quick freezing (liquid nitrogen), and indurative ones by excision
- “Cutaneous horns” indicate an area of dysplastic or even neoplastic epidermis, so such a horn is more likely a clinical marker of damage to the underlying epidermis than a diagnosis itself. These formations must be removed and sent for histological examination to assess changes in the underlying epidermis
- Bowen's disease is the clinical expression of cutaneous PCI in situ. It appears as an asymptomatic, well-circumscribed erythematous scaly patch that expands centrifugally. 8% of untreated cases develop invasive PCI
- In the past, it was unclear whether keratoxanthomas should be considered a benign or precancerous condition; Currently, the opinions of most experts are in favor of the latter. Treatment consists of curettage or wide excision and subsequent histological examination
Is cutaneous horn dangerous?
Cutaneous horn in humans, despite its benign nature, is a disease that requires treatment. After all, a tumor has a predisposition to degeneration. Therefore, if such a pathology is detected on the skin, it is recommended to treat it. Well, even in a “calm” state, it is better to remove the growth on the eyelid, lip, nose, since the formation significantly spoils the appearance. A conical growth 1-5 cm long attracts increased attention from others. This causes uncertainty, discomfort, and social withdrawal.
But let's return to the risks of malignant degeneration. This process occurs due to hereditary predispositions to the appearance of tumors. And the first symptom of danger is the appearance around the base of the growth of signs of inflammation and pain when touching the growth. It is better not to wait for such manifestations. Seek medical help if any pathology occurs. In our medical center you will receive qualified and professional care.
Frequent prerequisites for the formation of a neoplasm
The cause of the appearance of a cutaneous horn can be:
- hereditary predisposition;
- excess weight;
- excessive insolation;
- chronic stress;
- endocrine and metabolic disorders in the body;
- diseases of the gastrointestinal tract;
- vitamin deficiencies;
- viral skin infections (warts, condylomas, papillomas);
- the presence and chronic traumatization of senile and solar keratomas, papillomas, angiokeratomas, psoriasis, keratoderma, mucosal keratosis, lupus erythematosus.
Treating cutaneous horn at home
There are a dozen folk recipes that tell how to remove skin tumors. But you should not smear the skin with aggressive substances so that the horn falls off. Do not pull the growth or drip acid or alkali onto it. These tips carry health risks. Even if it is possible to remove the formation from the surface of the skin, the surrounding tissue can be seriously damaged. Also, the growth may not be completely removed, which will lead to relapse. And most importantly, it is impossible to conduct tissue histology at home. Therefore, it will be impossible to prevent the risks of degeneration at an early stage.
Diagnostics
When any neoplasm appears, its histological analysis should be carried out, which will determine the nature and further prognosis of the disease.
When this character is formed, it should not be confused with various types of warts, papillomas, and calluses. After a histological examination, a differential examination should be used to exclude the squamous cell form of skin cancer, for which a biopsy of a piece of tissue taken for analysis is performed.
The most vulnerable area of this neoplasm is considered to be its base - it is here that all the many processes occur that cause the pathological proliferation of tissues and the formation of a cutaneous horn. For a more detailed analysis, tissue is taken specifically from the base of the horn, which makes it possible to determine what type of neoplasm it belongs to - benign or malignant.
How to cure cutaneous horn?
For several decades, cutaneous horn removal was carried out only surgically. This method is quite effective. But after excision of the formation with a scalpel, scars and cicatrices almost always remain on the skin. This is a problem for patients whose cutaneous horn appears on open areas of the skin - on the face, on the neck, on the arms.
A modern alternative to surgery is laser removal of the skin horn. Laser therapy, especially in the early stages of pathology, has proven itself to be an effective and efficient way to completely, completely remove skin abnormalities.
The laser beam acts precisely and at the desired depth, so neighboring tissues are not damaged. The treatment is painless and long-term rehabilitation is not required. Since trauma to the skin is minimal, there are no scars or scars left on its surface. You can verify this by looking at photos of the skin of our patients before and after microsurgery.
It is important that there is no bleeding or inflammation at the site of micro-operation. After all, the laser beam cauterizes capillaries and tissues, preventing infection. The safety and painlessness of laser technologies allows them to be used not only in the treatment of skin pathologies in adults, but also in children. The method has only a few limitations. You can find out more about them at an appointment with a dermatologist at the Lasersvit Medical Center for Mole Diagnostics.
Prognosis and prevention
As a preventative measure, it can be recommended to avoid injury to the skin if possible, reduce the time spent in the open sun and the use of sunscreens when sunbathing, and also adjust your diet: according to doctors, it should contain a sufficient amount of vitamin C every day.
After removal of the growth, the prognosis is usually completely favorable. The malignancy of this neoplasm is no more than 5% of cases. Relapses of the disease are not often diagnosed.
Regular examination of your skin throughout the body will allow you to detect the onset of any pathological process in time; this is an important preventive measure, since the initial stage of any disease is easier to cure.
Be healthy!