Any external influence on the body, for example, a change in air temperature or contact with irritants, instantly affects the condition of the skin. Sometimes red spots and swelling appear on the body. The person experiences itching and burning.
Internal diseases and contact with aggressive chemicals can cause such symptoms. One of the common causes of itching and redness of the skin is allergies. Children are more likely to suffer from it. However, the body of an adult can also react inadequately to external irritations.
In a child, the cause of itching and redness of the skin on the body is often infectious diseases such as chicken pox or scarlet fever. The main symptoms are accompanied by hyperthermia, weakness, and general malaise. Infants often experience diathesis, in which the rashes are localized on the head, in the facial area, where crusts form. In the absence of therapy, weeping spots form in areas of redness. Typically, an allergic reaction is provoked by fruit juices and new complementary feeding mixtures.
The Rossimed clinic employs experienced allergists and dermatologists who can identify the cause of allergies and prescribe the necessary treatment.
Possible reasons
Overheating or hypothermia in people with hypersensitivity causes itching and redness of the skin. In winter, your hands and face suffer. Less commonly, areas covered by clothing. The skin may turn red from frost and wind, and small cracks may appear on it. This causes significant discomfort because it itches and flakes. This opens up the possibility of infection.
High ambient temperatures also cause itching and redness on the body. As well as direct exposure to ultraviolet rays. With prolonged exposure to the open sun, red spots appear on the body, then a small rash forms on them. Severe burns cause blisters. When overheated, body temperature rises to 37.2 degrees, nausea and vomiting are observed.
Neurodermatitis causes itching and redness of the skin, the causes of which are previous allergies. However, the disease develops in individuals with a hereditary predisposition, with a lack of vitamins and malfunctions of internal organs.
Neurodermatitis can occur due to overwork or stress. Patients suffer from unbearable skin itching and redness localized in the groin area, arms and legs, neck and head.
Fungal infections of the skin affect various parts of the body. Symptoms depend on the specific type of infection. Typically, areas of redness and swelling appear on the skin. Small lesions merge with each other and turn into plaques. The skin itches and flakes.
Psoriasis is a chronic disease that develops at a young age. The main reasons are psychological stress, poor nutrition, and vitamin deficiency. Plaques form on the scalp and body, covered with small white or silvery scales that peel off.
Other causes of red skin may be due to thyroid dysfunction. One of the symptoms of diabetes is itching and dry skin. These signs develop due to dehydration.
If a person suffers from itching and redness of the skin of the legs, then perhaps the cause is varicose veins of the lower extremities. In such a situation, scratching the damaged areas can lead to the formation of trophic ulcers.
In addition, similar symptoms may cause:
- Malfunctions of the central nervous system.
- Pathologies of the kidneys and liver.
- The presence of parasites in the body, for example, ticks, lice, worms.
- Blood diseases - anemia, varicose veins.
However, more often the symptoms in question are due to allergies.
The localization of lesions allows us to judge the reasons for the appearance of red spots on the body.
The face mainly suffers from poor cosmetics, poor quality tap water used for washing, and polluted air. The cause of irritation is sloppy shaving. Cold air causes the face to become chapped and cracks appear on it. Therefore, it is recommended to use a protective cream in winter.
Hands may become blotchy and itchy due to various internal diseases. For example, with liver pathologies and dysfunction of the thyroid gland, both the hands and other parts of the body itch - the stomach, neck, lower limbs.
In renal failure, a high percentage of urea accumulates in the blood serum, which causes itching. Neurodermatitis causes redness to form on the wrists, elbow joints and other bends of the arms.
Feet itch for various reasons. Unbearable itching is caused by fungal infections, varicose veins, cirrhosis of the liver and hepatitis. Affected areas of the skin can be observed on the lower extremities with psoriasis, bone diseases, endocrine and nervous system failures.
Make an appointment online
Sign up
How do redness appear in vascular diseases?
Varicose veins of the lower extremities are accompanied by swelling, which intensifies in the evening. If redness appears, then (attention!) it may already be thrombophlebitis. With thrombophlebitis, redness in the legs is accompanied by chills and fever, the skin turns red along the veins, and the veins themselves become denser.
At the MEDICUS clinic, leading specialists with extensive experience in solving such problems work with these problems. Choose the methods presented below and sign up using the online registration form.
Diseases
Food allergies develop when certain foods are consumed. These include all kinds of sweets, chocolate, citruses and exotic fruits, eggs, spices, pickles and pickled vegetables. Often there is no cure for food allergies. It is enough to remove provoking foods from the diet and the symptoms will disappear on their own. However, if signs of general intoxication appear - vomiting, nausea, diarrhea, you should consult a doctor.
In addition, some components of pharmacological drugs can be allergens. Rash and redness of the skin are caused by taking antibiotics. In severe cases, anaphylactic shock may develop.
Contact allergies occur when the skin is directly exposed to an irritant. Hygiene and household chemicals, cosmetics, and perfume can act as an allergen. Sometimes the cause of redness is tight shoes and items of clothing, for example, belts, elastic bands, straps. Jewelry and costume jewelry can cause irritation.
Stress as a cause of itchy skin. You can often notice that a person’s face turns red when very excited. However, with constant nervous tension, a rash may appear on the body, which itches and leaves significant discomfort. In addition to external medications, sedatives are prescribed in such situations. Sometimes serious psychotherapy becomes necessary.
Skin diseases in diabetes mellitus
Severe metabolic disorders underlying the pathogenesis of diabetes mellitus (DM) lead to changes in almost all organs and tissues of the body, including the skin. The etiology of skin lesions in diabetes is certainly associated with impaired carbohydrate metabolism and the accumulation of corresponding products of impaired metabolism, which leads to structural changes in the dermis, epidermis, follicles and sweat glands. In combination with diabetic polyneuropathy, micro- and macroangiopathies, impaired local and general immunity, this leads to the appearance of various types of rashes, age spots, ulcerations, as well as purulent-septic complications.
The skin of patients with diabetes undergoes peculiar general changes. In severe cases of the disease, it becomes rough to the touch, its turgor decreases, and significant peeling develops, especially on the scalp. Hair loses its shine. Calluses and cracks appear on the soles and palms. A pronounced yellowish coloration of the skin often develops. Nails become deformed and thicken due to subungual hyperkeratosis. Diffuse hair loss may be a symptom of poorly controlled diabetes.
Often, dermatological manifestations can act as “signal signs” of diabetes: itching of the skin, dry mucous membranes and skin, recurrent skin infections (candidiasis, pyoderma).
Currently, more than 30 types of dermatoses have been described, which either precede diabetes or develop against the background of a manifest disease. Conventionally, they can be divided into 3 groups:
- Primary - caused by diabetic angiopathy and metabolic disorders (diabetic dermatopathies, necrobiosis lipoidica, diabetic xanthomatosis, diabetic blisters, etc.).
- Secondary - fungal and bacterial infections.
- Dermatoses caused by drugs used in the treatment of diabetes (eczematous reactions, urticaria, toxicoderma, post-injection lipodystrophy).
As a rule, diabetic skin lesions have a long and persistent course with frequent exacerbations and are difficult to treat.
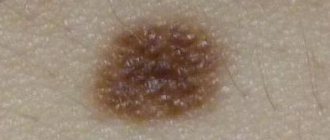
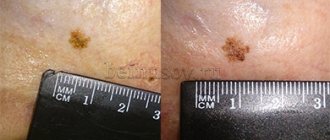
Diabetic dermatopathy. The most common lesion in diabetes is the appearance on the anterior surface of the legs of symmetrical reddish-brown papules with a diameter of 5–12 mm, which then turn into pigmented atrophic spots (more often detected in men with a long duration of diabetes). There are no subjective symptoms, the course is long, and they can disappear on their own within 1–2 years. Pathogenesis is associated with diabetic microangiopathy. There is no specific treatment for dermatopathy.
Diabetic bladder. Refers to rare skin lesions in diabetes. Blisters appear suddenly, without redness, on the fingers, toes, and feet. Dimensions vary from a few millimeters to several centimeters. The vesicular fluid is clear, sometimes hemorrhagic and always sterile. In most cases, blisters heal without scarring after 2–4 weeks of symptomatic treatment.
Rubeose. In childhood and adolescence, in patients with insulin-dependent diabetes, hyperemia in the form of a slight blush is observed on the skin of the forehead, cheeks (less often, chin), which is sometimes combined with thinning of the eyebrows.
Diabetic erythema. It occurs as ephemeral erythematous spots, which are observed mainly in men over 40 years of age who have had diabetes for a short time. These spots are characterized by large sizes, sharp boundaries, rounded outlines and a rich pink-red color. They are localized mainly on open skin - the face, neck, dorsum of the hand. Subjective sensations are either absent, or patients complain of a slight tingling sensation. The spots have a very short lifespan (2–3 days) and disappear spontaneously.
Acanthosis nigricans. It is characterized by villous hyperpigmented growths, mainly in the folds of the neck and armpit. Patients complain of “dirty skin” that cannot be washed. There are sometimes also small papules on the most prominent points of the finger joints. The pathogenesis is based on the liver's production of insulin-like growth factors, which interact with epidermal receptors and cause thickening of the epidermis and hyperkeratosis.
Diabetic xanthoma. It develops against the background of hyperlipidemia, with the main role played by an increase in triglycerides in the blood. Yellowish plaques are localized mainly on the flexor surfaces of the limbs, on the chest, face, neck and consist of an accumulation of triglycerides and histiocytes.
Necrobiosis lipoidica. A relatively rare chronic dermatosis characterized by focal disorganization and lipid degeneration of collagen.
Insulin-dependent diabetes is the most common cause of necrobiosis lipoidica and occurs in 1–4% of such patients. Skin manifestations may be the first - and for a long time the only - manifestation of diabetes. It is believed that in 18–20% of patients, necrobiosis lipoidica can occur 1–10 years before the development of typical symptoms of diabetes, in 25–32% of patients it develops simultaneously with this disease, but in the majority (55–60%) diabetes precedes skin lesions. There is no direct relationship between the severity of clinical manifestations of necrobiosis lipoidica and the severity of diabetes.
The disease can occur at any age, but more often it affects people between 15 and 40 years of age (mainly women). It occurs against the background of insulin-dependent diabetes and is characterized by large single lesions on the skin of the legs. The disease usually begins with the appearance of small bluish-pink spots or smooth flat nodules of rounded or irregular shape, prone to peripheral growth, followed by the formation of clearly demarcated, elongated oval or polycyclic indurative-atrophic plaques. Their central part (yellowish-brown) is slightly sunken, and the marginal part (bluish-red) is slightly raised. The plaques have a smooth surface, sometimes flaking along the periphery. Gradually, the central part of the plaques atrophies, telangiectasias, mild hyperpigmentation, and sometimes ulcerations appear on it. As a rule, there are no subjective sensations. Pain occurs with ulceration.
The appearance of the lesions is so characteristic that usually no additional research is required. In atypical forms, a differential diagnosis is made with granuloma annulare, sarcoidosis, and xanthomatosis.
There is currently no effective treatment. Drugs that normalize lipid metabolism are used (Lipostabil, Clofibrate, Benzaflavin); improving microcirculation (Curantil, Trental, Teonicol). Drugs such as Aevit, Dipromonium, Nicotinamide, Angiotrophin are indicated. Intralesional administration of corticosteroids, insulin, and Heparin is effective. Externally: applications of 25–30% Dimexide solution, application of Troxevasin, Heparin ointments, application of occlusive dressings with fluoride-containing corticosteroid ointments. Physiotherapy: phonophoresis of hydrocortisone, electrophoresis of Aevit, Trental. Laser therapy: for ulceration, surgical intervention is sometimes used (removal of lesions followed by skin grafting).
Itchy dermatoses (skin itch, neurodermatitis). They are often the first signs of diabetes. There is no direct relationship between the severity of diabetes and the intensity of itching. On the contrary: it has been noted that the most severe and persistent itching is observed in latent and mild forms of diabetes. In most patients, skin itching precedes the development of not only skin lesions in diabetes, but also the diagnosis itself (from 2 months to 7 years). Less commonly, itching develops against the background of established and treated diabetes.
The predominant localization is the folds of the abdomen, inguinal, intergluteal, and ulnar folds. The lesions are often unilateral.
Fungal skin lesions. The most common candidiasis is usually caused by Candida albicans. It is more common in old age and in obese patients with predominant localization of lesions in the genital area and large folds of skin, interdigital folds, mucous membranes (vulvovaginitis, balanopastitis, angular cheilitis). Candidomycosis may play the role of a “signal symptom” of diabetes.
Candidiasis of any localization begins with severe and persistent itching, which is later accompanied by objective signs of the disease. First, a whitish strip of macerated stratum corneum appears deep in the fold, and surface cracks and erosions form. The surface of the erosions is moist, shiny, bluish-red in color, bordered by a white rim. Around the main focus, “dropouts” appear, represented by small superficial vesicles and pustules. Opening up, these elements turn into erosions, also prone to growth and fusion. The diagnosis is confirmed by microscopic or cultural examination.
For local treatment, time-tested, simple and affordable means are used - alcohol or aqueous (the latter is better for large folds) solutions of aniline dyes: methylene blue (2-3%), brilliant green (1%), as well as Castellani liquid, ointments and pastes , containing 10% boric acid. Almost any local antimycotic can be used in the form of 1–2% creams, ointments, and solutions. External agents are used until the skin lesions are completely resolved, and then for another week. Systemic antimycotics include fluconazole, itraconazole or ketoconazole. Fluconazole is prescribed at a dose of 150 mg/day once; in case of torpid course, 150 mg/day once a week for 2–3 weeks. Itraconazole is prescribed at 100 mg/day for 2 weeks or 400 mg/day for 7 days. Ketoconazole is prescribed 200 mg/day for 1–2 weeks. The advisability of prescribing systemic antimycotics is determined by the effectiveness, previous therapy, the motivation of the patient who wants to get rid of the manifestations of the disease as soon as possible, as well as the availability of drugs.
Infectious diseases. Bacterial skin lesions occur in patients with diabetes much more often than in the general population and are difficult to treat. Diabetic foot ulcers are the most serious complication and can lead to amputation and even death.
Pyoderma, boils, carbuncles, cellulitis, erysipelas, paronychia and panaritium are most often caused by staphylococcal and streptococcal flora. The addition of infectious and inflammatory skin diseases, as a rule, leads to severe and prolonged decompensation of diabetes and increases the body's need for insulin. The diagnosis must be confirmed by obtaining a culture to determine sensitivity to antibiotics. The patient is prescribed oral dicloxacillin or erythromycin (if allergic to penicillin). Taking dicloxacillin is the main method of treating outpatients, since 97% of microorganisms are sensitive to it. Non-festering lesions can also be treated by applying heat locally. When fluctuating, the boil must be opened and drained. Large abscesses sometimes require incision and drainage.
In conclusion, it should be noted that skin lesions in diabetes are common conditions today, quite often encountered in clinical practice. Their treatment has certain difficulties and should begin with effective control of blood sugar levels and development of an adequate regimen for taking antidiabetic drugs. Without correction of carbohydrate metabolism in this group of patients, all therapeutic measures are ineffective.
Literature
- S. G. Lykova, O. B. Nemchaninova. Skin lesions in diabetes mellitus (pathogenesis, pathomorphology, clinical picture, therapy). Novosibirsk: Novosibirsk Medical Institute. 1997. 44 p.
- A. S. Mashkilleyson, Yu. N. Perlamutrov. Skin changes in diabetes mellitus // Bulletin of Dermatology and Venereology. 1989. No. 5. pp. 29–31.
- A. Yu. Sergeev, Yu. V. Sergeev. Fungal infections. Guide for doctors. M., 2003.
- I. I. Dedov, V. V. Fadeev. Introduction to Diabetology: A Guide for Physicians. M., 1998. 404 p.
- M. I. Martynova, E. E. Petryaykina, V. F. Pilyutik. Features of skin disorders in insulin-dependent diabetes mellitus. "Attending doctor".
I. B. Mertsalova, Candidate of Medical Sciences RMAPO, Moscow
How to prevent arthritis?
It is important to understand: there is not a single guaranteed way to avoid developing arthritis. It is not always possible to accurately determine the cause of the disease, which is why it is difficult to protect against it. You can only try to reduce the risk of arthritis and its complications.
- Follow a daily routine. Sleep at least 8 hours at night, during the day - according to your needs and capabilities. Adequate sleep strengthens the immune system and reduces the risk of developing infectious diseases - one of the causes of arthritis.
- Move more. Swimming, walking, yoga, gentle jogging, fitness - all this will benefit your joints.
Running with a partner is highly motivating
- Eat right. The diet should contain foods rich in polyunsaturated fatty acids (fish, vegetable oil), calcium and phosphorus (milk and dairy products). They strengthen the bone cartilage tissue of the joints. Add sources of vitamins to your daily menu - fresh fruits, vegetables, herbs. Reduce the proportion of fast carbohydrates and animal fats.
- Watch your weight. With obesity, the load on the joints increases, metabolism is disrupted, and the risk of arthritis increases.
- Get rid of bad habits. Quit smoking, limit your alcohol intake.
- Strengthen your immune system. There is no magic pill that can activate the body's defenses. Hardening and sunbathing will be beneficial. Eliminate stressful situations, don’t work too hard, take care of yourself.
- Don't get too cold. Dress for the weather, keep your feet warm, and maintain a comfortable room temperature.
Arthritis is a serious disease that can dramatically change your life for the worse. If you have swollen or reddened joints, pain or stiffness in movement, do not hesitate to visit a doctor. The sooner you start treatment, the easier it will be to slow down the progression of the disease and avoid complications.
Read also
Arteritis
Swelling and swelling of the arteries in the temple can be caused by temporal arteritis, a condition in which the temporal arteries, which supply blood to the skull and brain, become damaged and inflamed.
This… Read more
Fibromyalgia
“What is well recognized is well treated,” Hippocrates once said long ago and he was absolutely right, because only by understanding the cause and nature of the disorder in the human body can one successfully get rid of...
More details
Joint pain and swelling
Symptoms of joint pain and swelling can vary from person to person and depend on which joints are affected. Regardless of the cause, joint pain and swelling can cause significant...
More details
Rheumatoid nodules
Rheumatoid nodules are the most common dermatologic manifestation of rheumatoid arthritis (RA), occurring in approximately a quarter of patients with RA. Like other autoimmune diseases,...
More details
Joint pain and swelling, rheumatoid arthritis
Pain and swelling of the joints are a common cause of illness and impairment of the quality of life of patients. In this regard, the following types of joint diseases are distinguished: arthrosis (wear and destruction…
More details