Oral dermatitis is a local skin lesion, which consists of small papules (pimples), usually localized around the mouth, which determines the name of the disease. Another name for this disease is perioral dermatitis. Most often, this type of dermatitis is diagnosed in young women, less often in older women, but can also occur in children and teenage boys. Oral (perioral) dermatitis is an unpleasant cosmetic problem, which can still be eliminated if the cause of its occurrence is correctly identified and an effective treatment regimen is selected.
Medical is a clinic that diagnoses and treats many diseases, including dermatological ones. The treatment regimen in each specific case is selected individually, taking into account the characteristics of the patient’s body.
Clinical manifestations
Localization : has a characteristic location of the rashes, these are the perioral zone, nasolabial folds, skin of the chin and cheeks. The affected areas are characterized by symmetry.
Characteristic sign : a strip of healthy skin around the lips measuring 2-4 mm (characteristic in most cases, however, the case shown in the photo is a rare exception).
Rashes : pinkish-red papules, papulo-vesicles and papulo-pustules measuring 1-2 mm are located on an erythematous (red) background. Rashes are resolved by the appearance of crusts in place of the papules. The skin is dry, swollen.
Subjective sensations: characterized by a feeling of skin tightness, itching and burning.
Outbreaks of erythema with temperature changes, alcohol intake, spicy and hot foods. These manifestations are also characteristic of rosacea, which complicates the diagnosis of perioral dermatitis.
pigmentation may develop .
In what cases does perioral dermatitis occur?
The causes of perioral dermatitis are varied. During a detailed interview, the doctor tries to establish the cause of this condition in a particular patient, since further treatment depends on this. Most often, the development of the disease is associated with the following factors:
- prolonged and uncontrolled use of creams and ointments containing corticosteroids;
- the use of fluoride-containing products, for example the use of toothpaste with a high fluoride content;
- prolonged and uncontrolled use of products containing antibiotics;
- prolonged exposure to aggressive components included in some cosmetics and foundations;
- hormonal disorders.
Perioral dermatitis is similar to seborrheic dermatitis, rosacea and other skin diseases, so only a doctor can prescribe an accurate diagnosis and correct treatment. Therefore, only by seeking advice can you understand for sure that this is perioral dermatitis and receive the correct treatment regimen.
Manifestations of the disease
Perioral dermatitis can manifest itself in the chin, eyelids, corners of the lips, nasolabial and nasobuccal folds in the form of single papules, as well as in the form of extensive lesions. Papules are round, convex formations of red or pink color. There is itching and burning in the area of the rash. But there are also cases when papules do not cause any inconvenience other than aesthetic ones.
The affected areas of the skin feel uneven to the touch. In the area of papules, weeping may occur and crusts may subsequently form.
It is worth noting that most often papules form in the chin area and around the mouth rather than on the eyelids. There are also cases of mixed lesions, when papules spread over the entire face.
Possible negative consequences
If you do not seek medical help in time, wounds with pus may form in place of the papules. In this case, the percentage of affected skin will be much greater than at the beginning of the disease. Patients at particular risk are:
- with weakened immunity;
- with hormonal imbalance;
- childhood;
- with concomitant skin diseases.
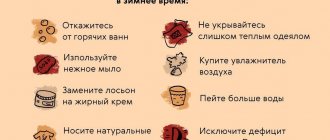
The course of dermatitis can worsen with the concomitant use of various medications, for example, hormonal contraceptives, as well as during pregnancy, when the skin is exposed to ultraviolet radiation, cold, wind, and dry indoor air.
Diagnosis of the disease
To accurately diagnose this type of dermatitis, you may need not only a doctor’s examination, but also additional manipulations, for example, scraping from the affected area of skin for microscopic examination, bacterial culture. Laboratory diagnostics may reveal:
- presence of demodex mite;
- increased microbial contamination of the skin;
- thinning of the skin with signs of inflammation based on biopsy results.
The difficulty can be considered the absence of a specific causative agent of perioral dermatitis, common for all patients, as well as nonspecific skin changes that may be present in other diseases.
Causes
The exact causes of the development of perioral dermatitis are not known, but trigger factors have been identified, i.e. provoking:
- Deterioration, weakening of immunity;
- Climate change;
- Exposure to ultraviolet rays;
- Use of corticosteroids;
- Fluoridated toothpaste;
- Genetic predisposition;
- The use of low-quality cosmetics against the background of a tendency to allergic reactions to cosmetics;
- Emotional stress.
The most reliable seems to be the development of perioral dermatitis in connection with long-term local use of corticosteroid ointments against the background of other provoking factors. There is a decrease in local immunity, which gives impetus to the development of the inflammatory process.
Risk groups and similar diseases
Signs of the disease are most often found in women, but children and adolescents periodically experience them due to weakened immunity. In place of the blisters, ulcers often form. When spread over the entire face, it becomes a threat to vision, which is especially important in the situation with children. Therefore, when checking with a specialized doctor about how to treat perioral dermatitis in children, it is worth paying a visit to an ophthalmologist.
In the case of teenagers, the disease may not be detected immediately, because, experiencing hormonal changes, boys and girls often encounter skin problems. Blackheads and acne affect most people, so it can be difficult to notice papules at an early stage. Patients prone to allergies also rarely accurately diagnose the disease. Perioral dermatitis in children is often attributed to hormonal imbalance.
Principles of therapy
For a pronounced therapeutic effect, an integrated approach is required in the correction of perioral dermatitis.
It is important to understand that the duration of therapy is quite long and takes from 6 to 8 weeks .
STAGE 1 – strict adherence to these recommendations
- Using fluoride-free toothpastes.
- If a course of external corticosteroids (hormonal ointments) was prescribed, complete use.
- Avoid the use of decorative cosmetics, especially in the rash area.
- Cleansing the skin only with specialized hypoallergenic products. For example, DermaQuest Cleansing Milk for Delicate Skin is designed for daily cleansing of dry, irritated, sensitive and dehydrated skin.
Heals dry and sensitive facial skin, giving the skin a feeling of comfort, cleanliness, and velvety.
- Compliance with a special dietary regimen that excludes the intake of hot, spicy foods and alcohol.
STAGE 2 – dermatological treatment
It is prescribed by a dermatologist after diagnosis and includes individual prescription of antihistamines, diuretics, sedatives, and sometimes antibiotic therapy.
Treatment of perioral dermatitis
Treatment of perioral dermatitis includes several stages.
Before treating perioral dermatitis , your doctor may recommend a complete detox of your skin and body. First of all, it is necessary to avoid the use of products that cause inflammation. Most often these are hormonal ointments, antibiotic creams or toothpaste with a high fluoride content. When you stop taking these medications, so-called “withdrawal dermatitis” may occur—burning and itching intensify, swelling and redness increase, and rashes literally “spread” all over the face. Such inconveniences can cause the patient to panic and desire to return the medications used to eliminate symptoms. However, this is the wrong path and will only make the situation worse. It is important to fully follow the doctor's instructions.
Since the skin is inflamed, during treatment it is necessary to avoid any products that could increase irritation. In particular, this applies to masking creams, powders, as well as cosmetics that are applied next to or directly on the area where perioral dermatitis appears.
Dietary instructions must also be followed. A diet for perioral dermatitis involves the complete exclusion of foods such as:
- alcohol;
- fast carbohydrates (industrial sweets, confectionery);
- smoked meats;
- hot spices, sauces;
- nuts;
- some types of fruits and vegetables.
Preference should be given to light vegetable dishes and light protein foods. When processing foods, preference should be given to steaming, boiling, stewing or baking.
To relieve the feeling of itching and burning on the skin, the doctor may prescribe antihistamines, and in particularly difficult cases, sedatives.
Skin-cap cream containing activated zinc pyrithione has shown effectiveness as a means for external treatment of dermatitis. The active substance (activated zinc pyrithione) helps eliminate inflammation, rashes, itching and excessive growth of microorganisms that increase inflammation. Skin-cap cream also contains neutral components that additionally moisturize the skin. The cream has a pleasant texture and helps eliminate the feeling of dryness and tightness of the skin.
In addition to the Skin-Cap medicinal cream, the doctor may recommend neutral skin cleansers and frequent irrigation of the affected areas with thermal water.
Effect of the drug
The antimicrobial ointment contains tetracycline hydrchloride. This substance destroys the cell membranes of many gram-positive and gram-negative microorganisms. In addition, the ointment is effective in the treatment of pathologies caused by other pathogenic microorganisms: gonococci, chlamydia, salmonella, pneumococci, etc. Tetracycline ointment, the instructions emphasize this, has no effect on viruses and fungi.
The principle of action of the external agent is to destroy the pathogenic focus, which allows stimulating restoration processes on the wound surface.
Composition and release form
Tetracycline ointment is produced in two types:
- 3% for external use in tubes of 5, 10, 30 or 50 g.
- 1% ophthalmic in tubes of 3, 7 and 10 g.
Antimicrobial ointment is yellow in color and has an oily structure. Aluminum or polymer tubes are packaged in cardboard packaging along with instructions for use. The active ingredient in its composition is tetracycline hydrochloride. In the production of tetracycline ointment, auxiliary components are used:
- Lanolin, which nourishes the skin and enhances the anti-inflammatory and regenerating properties of the ointment.
- Vaseline, which enhances the protective properties of the drug.
- Paraffin, which has softening properties and increases the viscosity of the product.
- Ceresin, used as a base and giving the ointment the desired consistency.
- Sodium disulfite, which is used as a filler.
Seborrheic dermatitis. Terminology
Seborrheic dermatitis
- a chronic inflammatory skin disease associated with an increase in the quantity and change in the quality of sebum, as well as with the influence of skin microflora.
The composition of sebum includes glycerides (more than 40%), free fatty acids (16%), wax esters (up to 25%) and cholesterol, squalene (12%) and cholesterol. Triglycerides in sebum are broken down into free fatty acids by bacteria. Some of them form volatile fatty acids that impart odor to the skin. Sebum itself has no odor.
The wide prevalence and constant increase in incidence determines various approaches to treatment, the main goal of which is to achieve a long-term positive result.
Manifestation of seborrheic dermatitis:
1) thickening of the stratum corneum, peeling;
2) oily sheen, seborrhea, sebostasis (stagnation of sebaceous secretion at the mouth of the hair follicle);
3) inflammation of the skin;
4) itching.
Seborrheic dermatitis affects those areas of the scalp and body where the sebaceous glands are most developed:
- scalp,
- anterior chest area and interscapular area,
- area of the ears,
- forehead,
- nasolabial triangle.
When the skin of the scalp is affected, thinning and thinning of the hair is observed. In severe cases, seborrheic dermatitis can have the character of a widespread exfoliative process up to erythroderma.
| Dandruff = seborrheic dermatitis | Brightness of blood vessels - inflammation |
Rules of application
Features of using the product:
- Tetracycline ophthalmic ointment, in a column no more than 1 cm long, is placed intraconjunctivally into the conjunctival sac (under the lower eyelid). A sterile stick is used for this. It is important to then distribute the product correctly using a cotton-gauze swab, performing gentle massaging movements.
- Ointment for external use 3% is applied to the affected areas of the skin in a thin layer. In this case, you need to capture a small area around the problem area. Additionally, a bandage is applied to enhance the therapeutic effect. If there is no damage to the skin, the product is practically not absorbed.
The course of treatment and its duration are determined by the attending doctor depending on the type of disease. For eye diseases, procedures are carried out 2-3 times a day. When using a 3% product to treat skin diseases, the dressing should be changed every 12-24 hours. Tetracycline ointment, the instructions for use provide this, can be used for acne. In this case, it is applied pointwise. The product can be used for 3 weeks in the absence of negative reactions from the body. If no improvement is observed within 2 weeks, then you should stop using the ointment and consult a doctor.
special instructions
The dangers of using tetracycline ointment during pregnancy are that the active substance can provoke processes of bone tissue mineralization, which increases the risk of developing bone abnormalities in the fetus.
It is not recommended to use the product for deep puncture wounds and other extensive damage to the skin, in particular after burns.
When using eye ointment for some time, the clarity of vision decreases. Therefore, after the application, you should not immediately drive a car. You should also be careful when performing work operations that require visual acuity.