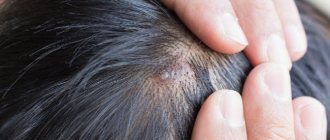
As a rule, atheroma occurs in those places where hair is developed. Therefore, the head, rich in sebaceous ducts, often acts as their incubator.
Atheroma on the head is caused by blockage of the sebaceous glands. The reasons are different - for example, as a consequence of injury or against the background of hormonal imbalance.
However, there is another reason. Remember the words of the heroine Ekaterina Vasilyeva from the movie “An Ordinary Miracle”: “What the hell do I need my head for when it hasn’t been washed for three days?” - she asks rightly. Yes, atheroma of the scalp can also occur due to the banal inability to keep hair clean.
Atheroma of the scalp can be congenital. This is a rare case when it can remain unchanged for many years. Or it may be acquired. Such atheroma occurs at any age and can literally grow from the size of a pea to the size of a chicken egg in just a matter of days.
!
In any case, atheroma is a disease that requires the attention of a doctor. And the sooner the better.
Firstly, the signs of atheroma are very similar to the symptoms of another neoplasm - lipoma; often only a professional diagnostician can distinguish them.
Secondly, a bump on the head attracts a lot of unhealthy attention.
In addition, a rapidly growing large atheroma resembles a cerebral hernia (brain prolapse). So, as is the case with any neoplasms, you cannot wait, nothing itself will ever resolve
!
Why does atheroma occur on the head?
Atheromas can be congenital or acquired. In the second case, their development is facilitated by:
- metabolic disorders,
- hormonal changes (high testosterone levels),
- poor hygiene,
- abrasions,
- increased skin oiliness.
Atheromas can be single or multiple, their sizes range from a pea to a chicken egg and larger. Since atheromas develop from the sebaceous glands, they occur more often on those parts of the body where there are many of these glands: on the head, face, neck, and armpits.
Reasons for development
It is still unclear why soft tissue sarcomas occur, but certain risk factors have been identified.
Genetic predisposition
- nevoid basal cell syndrome (Gorlin syndrome);
- neurofibromatosis (von Recklinghausen disease);
- tuberous sclerosis (Bourneville disease);
- Gardner's syndrome;
- Werner's syndrome.
Carcinogens
The risk of developing angiosarcomas increases significantly with previous exposure to phenoxy herbicides (2,4-dichlorophenoxyacetic acid, 2,4,5-trichlorophenoxyacetic acid) and dioxins.
Immunosuppression
The most striking example is Kaposi's sarcoma in people with AIDS, autoimmune hemolytic anemia, and organ transplant recipients.
Most patients come with a complaint of tumor growth after an injury or bruise. There is no connection between trauma and the development of soft tissue sarcomas.
Is scalp atheroma dangerous?
If there are no complications, then the biggest trouble that atheroma of the scalp causes is the lack of hair in the place where it is located. But the situation may change:
- If an infection gets inside the atheroma, it will turn into an abscess. An abscess of the soft tissues of the head will occur.
- Ulcers are dangerous on any part of the body, but especially on the head. The infection may spread deeper to form an intracranial abscess.
- Sometimes (although very rarely, there is such a possibility) atheromas transform into malignant tumors.
If an incomprehensible lump appears on the scalp, you should not wait for complications. Contact our doctors, they will remove it quickly and carefully!
What to do if warts appear on your head?
The likelihood that warts will disappear on their own in the near future is very low.
They do not go away even under the influence of mysterious spells, medicinal herbs or other methods that the boundless human imagination can come up with.
Perhaps the warts really are regressing.
But this can happen only in a few years, or even decades.
At the same time, they bother most people.
Even if the wart is overgrown with hair and is not visible, in any case it interferes with cutting and combing.
She is easily injured.
It may bleed, and sometimes the resulting wound festeres.
The wart should be removed.
This procedure does not cause pain, takes a few minutes and allows you to forget about the problem once and for all.
If a person does not see a doctor and is not treated, the wart may increase in size.
This does not pose a direct threat to health.
But subsequent removal requires treatment of a larger area of the head.
There is a higher risk that a scar will appear and hair in this area will no longer grow.
Therefore, it is better to remove a wart on the head earlier, while it is still small.
How are atheromas removed?
No amount of burdock, plantain or compresses with alcohol help with atheroma. It needs to be treated surgically. You should visit a doctor as early as possible. If the atheroma has festered, you need to run to the surgeon.
The most senseless way to remove scalp atheroma is puncture, when a needle is inserted into the cyst and its contents are pumped out with a syringe. No normal doctor does this (except perhaps to obtain the contents of the cyst and send it for a biopsy). As long as the walls of the atheroma are preserved, it will fill up again and again. In order to rid the patient of a cyst, its walls must be completely removed. The classic operation looks like this:
- Two bordering incisions are made on the skin in the area of atheroma.
- A blunt instrument (most often closed scissors) is placed under the atheroma.
- The atheroma is peeled off, and stitches are placed on the wound.
The intervention is performed under local anesthesia. Usually the operation is performed on an outpatient basis, but if the atheroma is large, hospitalization in a hospital may be required. However, scalpels are becoming a thing of the past. Surgeons now have more efficient tools. For example, lasers. With their help, atheroma on the head less than 5 mm in size can be evaporated without a trace; for larger ones, additional small incisions will have to be made.
An even more advanced way to remove atheromas of the scalp is radio wave and laser surgery. These are the methods that doctors at the ProfMedLab clinic use. Laser or high frequency radio waves work instead of a scalpel. They cause little tissue damage, healing occurs faster, and the cosmetic effect is better.
How to treat
Conservative treatment of atheroma without surgery is mostly a myth
. Traditional medicine cannot make a tumor disappear without a trace. So even an atheroma that has gone inside under the influence of Vishnevsky ointment will still appear again. In order to avoid a relapse of the unpleasant disease, the atheroma must be removed completely - along with the capsule around it. And only a surgeon can do this.
Therefore, at the first signs of the disease, you need to contact a plastic surgeon. Only this specialist will be able to not only remove atheroma on the head, but also make sure that the consequences in the form of scars and cicatrices do not overshadow your life in the future.
“Before” and on the 12th day after removal of myofibrolipoma of the forehead area. Tips&tricks on the forehead for faster resolution of swelling. Surgeon Vladislav Gladysheva.
Recurrence of atheroma after removal
Relapse is one of the possible complications after surgery to remove atheroma. Most often, the reason is trivial and related to the human factor: the doctor did not completely remove the capsule. We will consider the option when the surgeon did everything “perfectly”, and there was no trace of atheroma left on the head. Can it happen again? Maybe if the same thing happens to another sebaceous gland. Can this be prevented? Following three simple recommendations will help reduce risks:
- Wash your hair regularly and thoroughly.
- Use special shampoos that help fight oily scalp.
- Try to exclude fatty, sweet, and spicy foods from your diet.
If atheroma does appear, do not hesitate to visit a doctor. Make an appointment with a surgeon at the Medical Center: +7 (495) 120-08-07.
Classification
Classification by tissue from which tumor formation occurs:
- Fatty – liposarcoma;
- Muscular:
- striated muscle tissue - rhabdomyosarcoma,
- unstriated muscle tissue – leiomyosarcoma;
- Vessels:
- circulatory – hemangiosarcoma,
- lymphatic – linfangiosarcoma;
- Connective – fibrosarcoma;
- Synovial membrane – synovial sarcoma;
- Nervous – neurogenic sarcoma;
- Skin – fibrosarcoma.
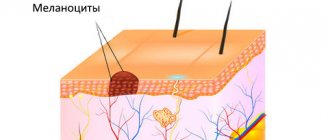
Hormonal causes of acne on the head
A failure in the production of one of the hormones in the human body can lead to malfunction of the entire system, including disturbances in the production of sebum on the head and the appearance of rashes, both abundant and not too much. In addition to acne, a number of factors can also indicate the presence of hormonal imbalance:
- absence of the menstrual cycle or its variability;
- a history of a diagnosis of polycystic disease or PCOS;
- Excessive male pattern body hair growth;
- painful menstruation;
- spotting outside the cycle;
- decreased libido and more.
The most common disorders in a woman’s hormonal system, which can cause acne on the head:
- insufficient function of the thyroid gland - hypothyroidism (with this diagnosis, less thyroid hormones are produced than the body needs);
- hyperfunction of the thyroid gland - hyperthyroidism (thyroid hormones are produced significantly more than the body needs);
- increased production of testosterone and the hormone DHEA;
- increased levels of prolactin in the blood serum;
- It is also necessary to control the level of insulin in the blood; if there is too much of it, metabolic processes in the body are disrupted.
There can be many reasons for dysfunction; high-quality diagnostics are needed to understand what to treat.
Examples of soft tissue sarcomas of the head and neck
Kaposi's sarcoma
Osteogenic sarcoma of the alveolar process of the maxilla
Osteogenic sarcoma of the mandible
Pleomorphic sarcoma of the soft tissues of the neck on the right
Diagnostics
The diagnosis is made based on histological examination of tumor tissue.
There are two methods for obtaining material for research:
- core needle biopsy;
- open biopsy.
The biopsy should be performed in the location that during the operation will be included in the area of excision of the tumor formation.
Diagnostic algorithm:
- Examination: A lumpy, rounded yellow or gray nodule may be observed. It can have different densities and consistencies. Soft nodes - with liposarcomas, dense - with fibrosarcomas, jelly-like formations - with myxomas;
- Complete blood count with calculation of leukocyte formula and platelet count;
- Biochemical blood test with determination of liver and kidney function indicators (including electrolytes);
- Coagulogram;
- MRI of the head and neck area;
- CT scan of the lungs;
- Ultrasonography;
- Radioisotope study of skeletal bones (for myxoid liposarcomas);
- CT scan of the brain (for alveolar soft tissue sarcoma and hemangiopericytoma).
Important: for the purpose of initial examination and clarification of the stage, routine PET scanning is not recommended.
Symptoms
Clinical manifestations and severity of symptoms depend on the primary location and size of the tumor.
Most often, soft tissue sarcomas of the head and neck are asymptomatic.
May be observed:
- pain;
- paresthesia is a disturbance of sensitivity along the course of peripheral nerves, which can manifest itself as burning, numbness, tingling;
- nerve palsies;
- trismus – spasm of the masticatory muscles, which is characterized by limitation of movements in the temporomandibular joint;
- ulceration of the mucous membrane;
- dysphonia is a phenomenon characterized by impaired vocal function;
- dysphagia – difficulty swallowing.
When soft tissue sarcomas are located near the nose, nasal congestion may occur that does not go away over a long period.
Prevention
Most often, hormonal imbalances occur in women due to the mobility of their hormonal system (every cycle a certain hormonal pathway occurs). To protect yourself from thinking: “What organ is wrong with me if acne appears on my head?”, women need to monitor their diet, sleep, be stress-resistant, and also not skip annual medical examinations.
Remember: it is better to prevent a disease than to treat it. And if you treat, then at the very beginning.
Treatment for a common process
Chemotherapy is the mainstay of treatment for advanced disease because the drugs injected enter the bloodstream and reach cancer cells throughout the body.
The most common chemotherapy drugs used for soft tissue sarcomas are doxorubicin, trabectedin, gemcitabine, docetaxel, and paclitaxel. These drugs may be prescribed alone or in combination.
Chemotherapy in patients with progressive disease should be based on doxorubicin or epirubicin, both drugs belong to the anthracyclines. In patients with angiosarcoma, paclitaxel or docetaxel may be offered instead of doxorubicin.
Adding another drug(s) to doxorubicin or epirubicin may enhance the effect of systemic chemotherapy in some patients. This choice primarily depends on the histological type of cancer.
If the first chemotherapy does not give the expected result, then another chemotherapy may be offered. The choice of one or more drugs will depend on previously used drugs, as well as on the histological type of the tumor. Drugs that may be considered include ifosfamide, trabectedin, gemcitabine, docetaxel, and paclitaxel.
Targeted therapy
This treatment works by binding to a specific protein or structure involved in tumor growth and progression. Side effects differ from traditional chemotherapy and depend on the mechanism of action of the drug. Targeted drugs approved for use in soft tissue sarcomas in Russia are:
- pazopanib – for soft tissue sarcomas other than liposarcomas;
- imatinib – for dermatofibrosarcoma, when systemic therapy is required.
Radiation therapy
Radiation therapy may be used to relieve symptoms or prevent complications, such as bone metastases.
Surgery
Surgical treatment of metastases may be considered depending on their location and medical history. For example, when lung metastases appear long after initial treatment and when, in the opinion of the surgeon, they can be completely removed.
Treatment
The treatment of a patient with sarcomas of the soft tissues of the head and neck requires an integrated approach with the involvement of a number of specialists: a morphologist, a surgeon, a radiation diagnostician, a chemotherapist, and a radiologist.
Surgery
Surgery is the main treatment method for patients with this pathology.
Soft tissue sarcomas grow within the capsule, which subsequently pushes away nearby tissue. This shell is called a pseudocapsule. Surgery involves removing the pseudocapsule en bloc with negative resection margins without damaging it, since violating the integrity of this formation increases the risk of tumor recurrence.
Postoperatively, radiation therapy may be administered to provide local control.
Additional treatments include chemotherapy and radiation therapy.
Radiation therapy
Preoperative radiation therapy provides significant advantages - the operating conditions are improved and the size of the tumor formation is reduced.
The negative aspect of this treatment is the high incidence of postoperative complications of an infectious nature.
Chemoradiation therapy
Treatment that combines chemotherapy with radiation therapy is called chemoradiotherapy.
Chemotherapy can improve the effectiveness of radiation therapy, so they are sometimes used together. This is a combination of systemic and local therapy.
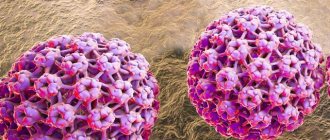
Treatment of papillomavirus infection
Papillomas are only a symptom, not a disease.
These symptoms are caused by the papilloma virus.
To prevent formations from reappearing after removal, treatment for papillomavirus infection is required.
It is carried out using:
- immunomodulators
- nonspecific (general action) antiviral agents
The drugs are used both locally and systemically.
They can be injected into the area where papillomas are located.
Systemic immunocorrection is also required.
It is usually performed by an immunologist under the supervision of an immunogram.
After normalization of immunity, the papillomavirus usually leaves the body within several months.