Moles are benign growths that are found on the skin of any person. Their number, location and size vary widely. Interestingly, it is impossible to find a single mole on a newborn’s body (the exception is congenital melanocytic nevi), and by adulthood their number usually reaches from 10 to 40, and can increase with age.
In medical parlance, moles are called pigmented nevi . They are benign neoplasms and are most often not dangerous. Under a microscope, they appear as clusters of melanocyte cells that produce the pigment melanin. The “evil twin” of a pigmented nevus is melanoma - this is a very aggressive malignant tumor that quickly grows into surrounding tissues, metastasizes, and in the later stages it is very difficult to fight.
In certain situations, moles can become a risk factor for melanoma:
- if a person has more than 100 pigmented nevi on his body;
- if dysplastic nevi are present, compared to ordinary nevi they are larger (more than 0.6 cm), irregular in shape, and have uneven coloring;
- Familial atypical nevus syndrome is a hereditary disease in which there are many dysplastic nevi on the skin;
- Congenital melanocytic nevi (those present from birth) develop into melanoma during life in 0–5% of cases.
Contrary to popular belief, melanomas do not always develop from benign nevi. In 70–80% of cases, they occur de novo, that is, in those places where there was previously unchanged skin. And only 20–30% of melanomas are former moles. Why this transformation occurs is not completely clear. Scientists continue to look for possible causes and risk factors.
By the way, there are mutations common to melanomas and pigmented nevi. For example, in nevus cells, in 68% of cases, the V600E mutation in the BRAF oncogene occurs, which leads to increased cell proliferation.
Many people intuitively perceive moles, especially large ones, as something not quite right, something that should not normally exist, and they try not to touch them again. You can often hear that a pigmented nevus should never be injured - otherwise it will turn into a malignant tumor. Many doctors also talk about this. Let's try to figure out how justified such fears are, and what we found out during scientific research.
Scientists' opinion
The most common malignant skin tumors are basal cell and squamous cell carcinoma. Everything has been clear with them for a long time: it has been proven that the likelihood of these tumors occurring is increased in those places where there are scars from severe burns and chronic inflammatory processes. Trauma contributes to the development of skin cancer and is one of the recognized risk factors. However, it is important to understand that although the risks are increasing, they are still very low. If you severely scald your hand with boiling water and you have scars, this does not mean that years later you will definitely develop a malignant tumor.
In the case of melanoma, there is no such clear evidence. Several studies have been conducted in the last century. Some of them describe cases where melanoma arose after injury to a mole or even “clean” skin. No other scientific work has found such a connection. Scientists are generally not inclined to make hasty conclusions; they are guided by the principle of post hoc ergo propter hoc - “after does not mean as a result.” If after a skin injury, either single or repeated, melanoma soon appears in that same place, this does not mean at all that the first entailed the second. There are also alternative explanations:
- Perhaps there was already a malignant tumor, and the injury simply forced him to pay attention to it.
- It is possible that the injury accelerated the growth of a pre-existing malignant tumor.
Let's consider another possible situation. A patient comes to a doctor to have a mole removed, and the doctor grants his wish. After some time, the mole grows back, it is removed again, and a biopsy shows that it is melanoma. Did the first operation provoke malignancy? It is impossible to give a definite answer to this question. Perhaps the patient originally had melanoma, and the first time it was not completely removed. Perhaps malignancy occurred later, and the operation had nothing to do with it.
In 2000, scientists from the University of Ulm (Germany) conducted a survey among 369 patients who were diagnosed with melanoma. 337 study participants said that no trauma preceded the appearance of a malignant tumor. 22 participants reported that they had previously experienced a single skin injury at the site of the malignancy, and 10 participants reported chronic skin injury. After conducting an analysis, the authors of the work came to the conclusion that, apparently, neither acute nor chronic skin injuries should be considered as causative factors in the development of melanoma.
In 2002, scientists from the National Cancer Center in Sofia (Bulgaria) conducted a case-control study, during which they surveyed 156 patients with melanoma and 156 healthy people. The authors concluded that trauma to benign pigmented lesions is associated with a slightly increased risk of melanoma, but this association was not statistically significant.
Of particular interest to scientists is the connection between injuries and the development of subungual melanomas, which occur under the nail plate. In this case, the role of the main risk factor for the development of melanoma, ultraviolet radiation, is not so high. Many scientists doubt that UV rays can penetrate the nail plates strongly enough to damage the DNA of the skin and lead to malignancy. In 2002, doctors from the Department of Dermatology at the University of Tübingen (Germany) decided to evaluate the role of mechanical injuries and analyzed data from 732 patients. Many patients noted that the development of the tumor was preceded by trauma to the fingers or toes, however, it was not possible to assess whether there was a real connection. The authors of the work suggest that trauma forces attention to melanoma or somehow contributes to its growth. It should be noted that subungual melanoma is generally quite difficult to diagnose; doctors often detect them in the later stages. Injuries to fingers and toes are by no means uncommon, especially among people who engage in physical labor or sports. At the same time, subungual melanoma is rare; in Europeans it accounts for 2–3% of all cutaneous melanomas.
There are still more questions than answers. One way or another, there is not a single case known in which it was possible to prove an unambiguous cause-and-effect relationship between skin damage and the development of melanoma. But such a connection cannot be completely ruled out.
Medical classification of melanomas
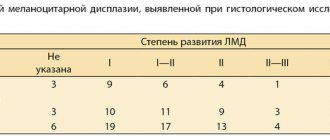
To determine the stage of melanoma, the Unified Staging System is quite informative, which distinguishes 4 stages - according to the thickness of the tumor and the depth of its invasion according to Clark:
- 1 – tumor thickness up to 1.5 mm with invasion level 2-3;
- 2 – tumor thickness up to 4 mm and invasion level 4-5;
- 3 – regional presence of metastases about 3 centimeters in diameter;
- 4 – distant metastases.
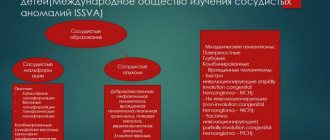
Melanoma can occur in both cutaneous and extracutaneous forms (10-20%) - with localization on the mucous membrane of the esophagus, rectum, genitals, eye mucosa, etc. The proportion of cutaneous forms is incomparably greater - 70-80%, but poses no less a threat for a large number of people around the world.
Cause for concern
Modern scientists are finding more and more similarities between the processes that occur during chronic tissue damage and in malignant tumors. In fact, this idea is not new. Even the German pathologist Rudolf Virchow, who lived in the century before last, called cancer an “unhealing wound.” When tissue damage occurs as a result of mechanical injury or inflammation, active regeneration processes begin in it. Certain types of leukocytes rush to the lesion. They secrete biologically active substances that cause cells to actively multiply. Genes that normally should not work are temporarily “turned on” in cells. And this can contribute to the development of a malignant tumor. For example, the role of chronic inflammatory process in the development of stomach and intestinal cancer has been established.
Perhaps this concept can explain why 20–30% of patients develop melanoma from pigmented nevi. According to the “unhealed wound” theory, moles can become malignant not only due to defects in the DNA of melanocyte cells, but also due to processes occurring in the surrounding tissues. And these processes, in turn, can be the result of inflammation or injury.
In 2015, a team of scientists from the UK and Denmark conducted an experiment on zebrafish and obtained very interesting results. These fish, like humans, can develop melanoma, their immune systems work in much the same way, and their transparent larvae are easy to observe. Over the course of several months, the researchers cut off the fish's tail fin in the same place every two weeks. And these repeated injuries increased the rate of development of malignant tumors.
This study does not prove that an accidentally damaged mole in a person will develop into melanoma, but it does suggest the possibility. Dr. Philip Niethammer from the Memorial Sloan-Kettering Cancer Center (USA) notes some weaknesses of the study by European colleagues:
- Although the results of the zebrafish experiment look very convincing, they cannot be completely extrapolated to humans.
- The intervention of scientists during the experiment is too far from real life. The researchers cut off the fish's fin in the same place many times. It is unlikely that a person will pick off the same mole over and over again. Although, in some cases, similar repetitive injuries can occur - for example, during shaving in men, if the mole is on the face.
- It is unclear whether a single injury can have the same effect as repeated injury. This possibility cannot be ruled out, but there is no evidence yet.
So, while doctors and scientists cannot say for sure whether mechanical trauma to a mole can lead to the development of melanoma. To get a definite answer, additional research is needed. For now, I can give only one piece of advice: it’s better not to touch moles, just in case. Nevi that constantly rub against clothing or are damaged during shaving are probably worth removing - although no one can say that constant trauma increases the risk of their malignancy.
Book a consultation 24 hours a day
+7+7+78
Symptoms of degeneration
Signals for the transformation of a nevus into a cancerous tumor can be as follows:
- bleeding;
- peeling, cracking of the skin;
- the appearance of compactions, nodules;
- the appearance of volume (the mole begins to rise above the skin);
- unpleasant sensations in the nevus area (pain, burning, itching).
If these signs appear, it is necessary to check moles for cancer.
Oncology specialists will conduct a full examination of the skin, including moles that cause concern. At the medical center, diagnostic activities are carried out using modern equipment. We are located at: Moscow, 2nd Tverskoy-Yamskaya lane, 10. You can make an appointment using the feedback form or by phone.
Diagnostics
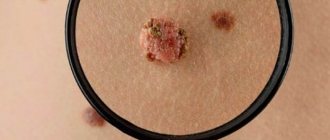
If a papilloma formation is detected on a mole, you must seek help from a specialist. First of all, the doctor will collect the necessary information regarding the patient’s medical history, the time when the growth of an additional tumor was noticed, and what symptoms accompany the process.
After this, a visual inspection of the affected area is carried out, which allows you to determine the size and color of the growth.
If this data is insufficient, an additional diagnostic examination is carried out, including several methods:
- biopsy - necessary to take a fragment of the affected tissue;
- histology – a histological examination of a previously taken sample of material is carried out to determine the nature of the neoplasm and the mole itself on which it appeared, which makes it possible to determine the degree of malignancy of the pathological process;
- PCR diagnostics to detect urogenital infection.
Also, if necessary, a laboratory blood test can be performed, which will also show some deviations from the norm in the presence of the disease.
Could it be a wart or other formations?
There are two types of age spots: congenital and acquired.
Acquired moles may develop warts or papilloma. There are characteristic features that distinguish nevus from other growths.
The following is considered normal:
- the presence of a light brown or dark brown tint;
- round or oval shape with clearly defined edges;
- size up to 10 millimeters.
Description of a benign formation that does not pose a health hazard.
Description
Papillomas on the surface of a mole are an ambiguous phenomenon that requires careful study and diagnostic measures.
A nevus (mole) is a benign formation, which, as an independent manifestation, is harmless to the human body. Its structure is made up of special cells - melanocytes, arranged in layers.
Inside the cavity there are follicles, sweat and sebaceous glands. However, the basal epithelial layer is absent. It is from this that the formation of papillomas occurs.
What does papilloma look like?
Papilloma is a benign neoplasm that appears on the body when infected with papillomavirus.
This neoplasm is benign in nature, but differs in the nature of its origin. The development of papillomas occurs when infected with human papillomavirus.
The growth may be light pink or flesh-colored. The shape resembles a nipple on a stalk, rising above the surface of the skin. Has a predisposition to increase in length.
Consists of a loose, soft structure and choroid plexuses. The diameter can reach from 2 to 15 millimeters. As a result of injury, its rapid growth is noted.
When exposed to certain factors, various changes can occur in the body, against the background of which a condition is observed when a papilloma grows from a mole.
If such a phenomenon occurs, you need to worry. Separated from each other, these neoplasms do not pose a danger to human health. But when a papilloma begins to grow from a mole, it may indicate cellular dysplasia.
Prevention
To avoid possible risks, you need to be careful about your skin. First of all, this applies to people who have fair skin, blue eyes and a lot of freckles on their body. It is this category that is more susceptible to cancer processes.
To avoid the growth of moles and the formation of papillomas on them, it is not recommended to spend a lot of time under the sun. Equally important is proper nutrition and healthy lifestyle.
Moles and papilloma individually are not dangerous to human health. However, if a papilloma growth is formed from the nevus itself, then in this case you need to be extremely careful, and it is better to consult a doctor, since such a condition may signal a possible process of malignancy.
Causes
The main provoking factor in the formation of a neoplasm on a nevus is the penetration and activation of the human papillomavirus.
Infection is possible in several ways:
- injury (infection enters the body through scratches, cuts, microscopic cracks);
- unprotected sexual contact with a person who is a carrier of an active virus;
- use of general hygiene products (washcloth, soap, towel, etc.);
- transmission of a viral infection from mother to newborn during passage through the birth canal.
In addition, papilloma can occur as a result of its damage, especially if the nevus is hanging or convex.
Treatment methods
The tactics of therapeutic measures will depend on the results of the examination.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
You just have to remember that treatment should be carried out in a complex manner. It is mandatory to prescribe a course of antiviral drugs, as well as medications that help increase and strengthen the patient’s immune system.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
To remove papilloma on a mole, doctors can use several methods.
Traditional surgery
This surgical technique is used if the papilloma in diameter exceeds more than one centimeter, or if the development of an oncological process is suspected.
The procedure consists of complete excision of the tumor along with the nevus on which it formed, as well as uninjured areas of the skin. This effect reduces the risk of relapse, that is, the reappearance of tumors.
Laser therapy
Refers to low-traumatic techniques. It involves influencing the growth using a laser beam. This tactic is used when formations appear that do not exceed five millimeters in diameter.
Cryodestruction
The procedure is carried out using liquid nitrogen. Under the influence of low temperatures, the papilloma freezes and will be removed. This technique is not recommended for getting rid of papillomas on moles localized in the facial area, as it has a number of side effects.
These include swelling of the treated area, death of hair follicles, and increased pigmentation.
Electrocoagulation
High frequency waves are used. Using the procedure, you can remove the formation, as well as immediately take a sample of pathological tissue for further cytological and histological examination.
Radiotherapy
Removal of moles with papilloma is carried out under the influence of a radio wave scalpel. It can be used in the formation of multiple papillomas, as well as if they are located on the genitals.