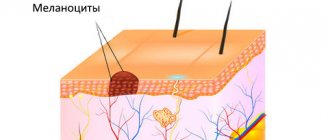
Blue nevus or Jadassohn-Tiche blue nevus (medical name) is a benign neoplasm of dense texture, about 1 cm in size. Outwardly, it looks like a dark blue or light blue nodule. The color of the formation is due to the accumulation of melanin in the layers of the skin. The color may be uneven, darker towards the center. The formation is elastic and mobile, has a smooth surface and does not cause painful sensations on palpation, and is not accompanied by itching.
Blue nevus is usually a single formation. But in rare cases, patients are diagnosed with multiple skin pathologies. The neoplasm is not a congenital anomaly. This mark can appear at any age. The most common places are the face, legs, hands, neck and buttocks. However, the anatomical location does not play a role in the prognosis of the development of the disease. Unless, due to its physiological location, the formation is subjected to regular traumatic mechanical action.
Why does blue nevus appear?
The true reasons for the appearance of this melanocytic formation have not been studied. It is only known that the nature of the skin abnormality lies, as mentioned above, in the accumulation of cells that produce melanin. As for the predisposing factors of its appearance, doctors include:
- hormonal changes (this type of formation appears during puberty; blue nevus is diagnosed in a child extremely rarely);
- unfavorable environmental situation;
- excessive solar radiation, frequent visits to the solarium.
The melanocytic formation, called “benign melanoma,” behaves quite calmly. However, today doctors recommend not observational tactics, but removal of the blue nevus even before the first signs of degeneration appear. This helps prevent skin cancer.
Removal of Jadassohn's nevus in young people
T. A. Gaidina (1, 2), A. S. Dvornikov (1), P. A. Skripkina (1), G. B. Arutyunyan (1)
Relevance of removal of Jadasson's nevus in young people
(1) Department of Dermatovenereology, Faculty of Medicine, Russian National Research Medical University named after N. I. Pirogov, Moscow
(2) Rednor Company LLC, Moscow
One of the benign skin formations is seborrheic nevus of Jadassohn (NSJ) - a hamartoma localized primarily on the skin of the face or scalp and is equally common in men and women. Pluripotent primary epithelial cells included in the structure of the NSJ are a favorable environment for the development of both benign and malignant tumors against its background. To exclude neoplastic transformation, it is advisable to remove the NSJ immediately after puberty. If surgical intervention is not possible, patients require constant dynamic monitoring. This paper presents two cases of successful CO2 laser removal of NSJ in young patients.
Key words: seborrheic nevus of Jadassohn, benign skin formations, malignant transformation of nevus, removal with CO2 laser
In 1895, the German dermatovenerologist Joseph Jadassohn first described hamartoma of the sebaceous glands [1]. Nevus of the sebaceous glands of Jadassohn (syn.: Nevus sebaceous Jadassohn, NSJ, nevus of the sebaceous glands, seborrheic nevus) is a congenital organoid nevus, localized primarily on the skin of the face or scalp and is equally common in both sexes (Fig. 1). The development of nevus is caused by proliferation and malformation of the sebaceous glands and is the result of differentiation of pluripotent cells towards mature sebaceous and apocrine structures [2]. Clinically, NSJ is presented as an asymptomatic solitary plaque of a round or linear shape, slightly raised above the skin level, up to 10 cm in size and has small hemispherical papules of pink, yellow or brown color with a smooth or papillomatous surface. NSJ is characterized by age-related features associated with the differentiation of sebaceous and sweat glands [3]. In young children, the nevus is hairless, hardly noticeable and has a smooth or poorly defined papillary surface. During puberty, the NSJ becomes more convex and becomes covered with closely adjacent papules, the color of which varies from light yellow to dark brown. Histological examination of NSJ in older patients can reveal abnormal formation of the epidermis and lobules of mature pilosebaceous follicles, a large number of different epithelial structures (dilated apocrine glands, abortive hair follicles) [4]. In adolescents, there are accumulations of undifferentiated cells resembling foci of basal cell carcinoma [2].
Fig.1
Seborrheic nevus of Jadassohn on the skin of the cheek in a 35-year-old woman.
This paper describes two clinical cases of removal of Jadassohn's sebaceous nevus using a CO2 laser.
Description of clinical cases
Case 1
Patient K., an 18-year-old man, came to the clinic with complaints of a formation localized on the skin of the left half of the bridge of the nose (Fig. 2).
Fig.2
Patient K., 18 years old. Seborrheic nevus of Jadassohn with cutaneous horn on the skin of the dorsum of the nose. Side view
History: the patient had the formation since birth. During puberty, he began to notice its slight growth and scanty discharge of a light yellow color, appearing when pressed. The young man repeatedly tried to independently squeeze out and remove the formation that was annoying him. A year ago, a growth appeared in the center of the formation, which over the past 6 months has increased to 0.5 cm (Fig. 3).
Fig.3
The same patient. Seborrheic nevus of Jadassohn with cutaneous horn on the skin of the dorsum of the nose. Front view
Status localis: the skin of the face is of normal color, in the T-shaped zone there is excessive sebum secretion, closed comedones. On the skin of the left half of the dorsum of the nose there are papules merging into an oblong-oval plaque measuring 0.5 × 0.8 cm, light pink in color, having a lobular structure and slightly rising above the skin level. In the center of the formation there is a cylindrical outgrowth 0.1 × 0.1 cm at the base and 0.5 cm in height. At the top of the outgrowth there are dense layered horny masses. On palpation, the formation is soft and painless. Histological examination: papillomatous epidermal hyperplasia and hyperplasia of the sebaceous glands were revealed. Clinical diagnosis: D23.3, seborrheic nevus of Jadassohn, cutaneous horn. Taking into account the localization and small size of the formation, a decision was made to remove the formation with a CO2 laser under local anesthesia. Examination 2 weeks after removal showed the formation of a normotrophic scar (Fig. 4)
Fig.4
The same patient. Formation of a normotrophic scar after removal of Jadassohn's nevus with a CO2 laser
Case 2
Patient A., a 30-year-old woman, came to the clinic for the aesthetic correction of a formation on the skin of her forehead (Fig. 5). History: the patient had the formation since birth. During puberty, the formation slightly increased in volume, became more protruding above the surface of the skin and acquired a darker color. Over the past ten years, the patient has not noted any changes.
Fig.5
Patient A., 30 years old. Seborrheic nevus of Jadassohn on the forehead.
Status localis: facial skin of normal color. On the skin of the forehead there are papules that merge into an oblong-oval plaque measuring 1.7 × 1.1 cm, light brown in color with a bumpy surface. The formation is characterized by a lobular structure and rises slightly above the skin level. On palpation it is soft and painless. Histological examination: subepithelial proliferation of the sebaceous glands was revealed (Fig. 6).
Fig.6
Skin fragment with subepithelial proliferation of sebaceous glands. Staining: hematoxylin-eosin; magnification x40.
Clinical diagnosis: D23.3, seborrheic nevus of Jadassohn. The patient underwent removal of the formation with a CO2 laser under local anesthesia. Examination 2 weeks after removal showed the formation of a normotrophic scar (Fig. 7).
Fig.7
Patient A., 30 years old. Formation of a normotrophic scar after removal of Jadassohn's nevus on the forehead skin using a CO2 laser
Discussion of clinical cases
There are differing opinions regarding the timing and advisability of NSJ removal. Before puberty, the NSJ is usually not noticeable. After puberty, secondary benign neoplasms develop in the NSJ with a frequency of 10–30% [5]. The literature describes various benign tumors that develop in the NSJ, of which trichoblastoma and syringocystadenoma are the most common [6]. This transformation of the NSJ brings additional discomfort to patients and requires aesthetic correction. The development of cutaneous horn due to NSJ is a rare phenomenon [7, 8]. There are no exact statistics on the incidence of malignant transformation of NSJ. The rarity of malignant transformation is noted by domestic researchers [2] and some foreign sources [9]. Other authors indicate malignant transformation in 22% of cases [10], most of which are described in patients over 50 years of age [11, 12]. It has been proven that the risk of malignant transformation increases with age [11]. Cases of the development of multiple neoplasms within the same NSJ in people over 50 years of age have been described [13]. The typical localization of NSJ on the skin of the face and scalp is also one of the risk factors for degeneration into a malignant tumor type. The cellular structure of NSJ (pluripotent primary epithelial cells) serves as a favorable environment for the development of malignant neoplasms against its background [2, 4]. Considering that the risk of malignant transformation exists, and the presence of the nevus itself is accompanied by aesthetic problems in patients, the authors consider it advisable to remove the NSJ in patients after puberty. The choice of removal method in young patients is quite wide: curettage, cauterization, cryotherapy, photodynamic therapy, laser ablation, surgical excision. The experience of successful use of a CO2 laser with a good cosmetic effect has been described in children [14]. This method is characterized by high efficiency, less damage to normal tissues and good cosmetic effect. In patients over 50 years of age, removal should be performed by radical surgery. If it is impossible to do this for any reason, constant dynamic monitoring is indicated.
CONCLUSIONS
The presented clinical cases demonstrate a good cosmetic effect after removal of NSJ with a CO2 laser. This method can be recommended as the method of choice for removing NSJs up to 2–3 cm2 in size in young people.
Literature
1. Lantis S, Leyden J, Heaton C. Nevus sebaceous Jadassohn. Arch Dermatol 1968, 98:117–23.
2. Molochkov V. A., Mardi Sh. On the development of basal cell carcinoma against the background of Jadassohn’s nevus of the sebaceous glands. Almanac of Clinical Medicine. 2007; 15:232–5.
3. Simi C, Rajalakshmi T, Correa M. Clinicopathologic analysis of 21 cases of nevus sebaceus: A retrospective study. Indian J Dermatol Venereol Leprol. 2008; 74 (6): 625–7.
4. Alessi E, Sala F. Nevus sebaceus. A clinicopathologic study of its evolution. Am J Dermatopathol. 1986; 8 (1): 27–31.
5. Liu Y, Valdebran M, Chen J, Elbendary A, Wu F, Xu M. Nevus sebaceous of Jadassohn with eight secondary tumors of follicular, sebaceous, and sweat gland differentiation. Am J Dermatopathol. 2016; 38(11):861–6.
6. Jaqueti G, Requena L, Sánchez Yus E. Trichoblastoma is the most common neoplasm developed in nevus sebaceus of Jadassohn. A clinicopathologic study of a series of 155 cases. Am J Dermatopathol. 2000; 22 (2): 108–18.
7. Pointdujour-Lim R, Marous MR, Satija CE, Douglass AM, Eagle RC, Shields CL. Cutaneous Horn of the Eyelid in 13 Cases. Ophthalmic Plastic and Reconstructive Surgery. 2017; 33 (4): 233–6.
8. Arvas L, Livaoglu M, Karacal N, Sozen E, Kara B. Giant cutaneous horn with naevus sebaceous. J Plast Reconstr Aesthet Surg. 2007; 60 (11): 1268–9.
9. Kamyab-Hesari K, Seirafi H, Jahan S, Aghzadeh N, Hejazi P, Azizpour A, et al. Nevus sebaceus: A clinicopathological study of 168 cases and review of the literature. Int J Dermatol. 2016; 55 (2): 193–200.
10. Westfried M, Mikhail GR. Multifocal Basal-Cell Carcinomas in a Nevus Sebaceus of Jadassohn. J Dermatol Surg Oncol. 1981; 7 (5): 420–2.
11. Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: A study of 707 cases. J Am Academ Dermatol. 2014; 70 (2): 332–7.
12. Jardim MML, Souza BC, Fraga RC. Rare desmoplastic trichilemmoma associated with sebaceous nevus. Anais Brasileiros de Dermatogia. 2017; 92(6):836–7.
13. Liu Y, Valdebran M, Chen J, Elberdary A, Wu F, Xu M. Nevus Sebaceous of Jadassohn wiht Eight Secondary Tumors of Follicular, Sebaceous, and Sweat Gland Differentiation. Am J Dermatopathol. 2016; 38(11):861–6.
14. Ashinoff R. Linear Nevus Sebaceus of Jadassohn Treated with the Carbon Dioxide Laser. Pediatric Dermatol. 1993; 10(2):189–91.
RUSSIA NEWSLETTER | 3, 2022 | VESTNIKRGMU.RU
Types of blue nevus
Blue nevus of the skin is classified by experts as follows:
- A simple (vulgar) blue nevus is characterized by a smooth surface and the presence of a nodule in the center. When studying the formation, fibroblast-like cells with different melanin contents are found, grouped into irregularly shaped bundles. The joints are surrounded by fibrous tissue and lie at different levels of the skin.
- Cellular blue nevus has a darker color and a rough surface texture. When examined, the formation demonstrates a predominance of “strands” of spindle cells in the stroma. Because of this feature, it is often confused with a malignant skin tumor.
- Mixed or combined nevus received this name for the presence of characteristic features of the two listed types of neoplasm. The skin anomaly has uneven edges and can lie in both the superficial and subcutaneous layers.
For patients, this information may be useful because cellular blue nevus and the combined type of formation are more likely to degenerate. And only a dermatologist can determine the form of the pathology during a comprehensive examination.
Symptoms of blue nevus
Blue nevus can appear in people of any age group, but most often it is first discovered in middle age. It usually does not cause patients any particular discomfort (except for a cosmetic defect when it is localized on the face and is large in size). Blue nevus has the following clinical characteristics:
- intradermal nodule;
- round, spindle-shaped or elliptical shape;
- light gray, dark blue, blue-black or blue color;
- uneven color;
- clear contours;
- smooth, hairless surface;
- the size rarely exceeds a centimeter (although there are blue nevi larger than 3 cm);
- protrudes slightly above the skin or does not rise above it at all;
- the consistency is elastic and dense;
- most often localized on the buttocks and limbs;
- can form on the mucous membranes of the mouth, vagina, and cervix.
Is blue nevus dangerous?
Due to its appearance and color, the growth is often compared to melanoma. Benign quality can be confirmed by:
- even color;
- symmetrical shape;
- undamaged surface without cracks or ulcers;
- absence of discomfort, pain, itching.
A blue nevus is dangerous if it begins to grow rapidly. Concerns can be caused by peeling of the surface of the neoplasm, changes in color uniformity, and the appearance of new nodules in the “body” of the nevus. Also, the tissue around the problematic pigmented mole may become red and swollen. If you discover these symptoms in yourself, if you experience discomfort or pain when touching the tumor and even without it, you should immediately visit a dermatologist’s office to diagnose the pathology. It is important to remember that melanoma is an aggressive cancer with a rapid progression. And the factors provoking degeneration are:
- frequent mechanical damage to the formation;
- ultraviolet (solar) irradiation;
- decreased immunity, stress;
- hormonal disbalance.
Not a single doctor can say with a 100% guarantee whether a blue nevus of the skin will degenerate or not. Therefore, it should definitely be observed, and it is better to remove it to eliminate the risk of developing skin cancer.
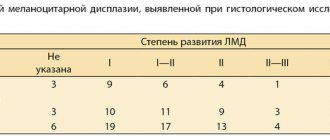
How dangerous are dysplastic nevi?
There are specific, proven figures here that it would be better for those who spread hysteria on the “Internet” to become familiar with.
- The annual risk of a dysplastic nevus turning into melanoma is 1 in 10,000. According to the authors [4], this is very low.
- About 70% of melanomas develop not against the background of nevi, but against the background of unchanged skin [5].
- A study examining the genetic profile of atypical nevi has challenged the hypothesis that they are precursors to melanoma [6].
- In two studies, the authors followed patients with incompletely removed, histologically confirmed dysplastic nevi for a long time (up to 17 years) [8,9]. Based on this, the very thesis about the increased risk of developing melanoma from a dysplastic nevus can be seriously questioned.
Diagnosis of blue nevus
Diagnosis of education is carried out using special equipment. Diagnostic techniques such as dermatoscopy, spectrophotometric intracutaneous analysis, histological examination, and sometimes ultrasound are practiced.
They make it possible to study the boundaries and uniformity of melanin distribution in the spot, the depth of the tumor, and the cellular structure. After diagnosis, the doctor gives competent recommendations for further treatment of the skin abnormality.
Congenital melanocytic nevus - symptoms and treatment
For congenital nevi, surgical and drug treatment, laser therapy and other methods are used.
Surgery
Large nevi are recommended to be removed in early childhood - this will help avoid emotional and behavioral disorders in the child. Such children, due to external differences, may consider themselves inferior to others and avoid their peers. In addition, they may face bullying from other children.
However, not all nevi can be completely removed. If they occupy a large area and the defect cannot be closed with healthy tissue, then the operation is not performed, or the nevus areas are partially excised.
The extent of the operation depends on the location of the nevus and the depth of the lesion. Its necessity for large and giant nevi is considered controversial. Many experts suggest removing the most heterogeneous, thick or coarse areas of the nevus, which complicate clinical observation [45][46]. Often the best choice is to closely monitor the nevus without undergoing surgery.
The only absolute indication for surgical treatment is the development of a malignant tumor in the lesion. But even with complete excision of large and giant nevi, the risk of oncology remains, since melanocytes can penetrate deep-lying tissues: muscles, bones and the nervous system.
The following complications may occur after surgery: contractures, seromas, hematomas, soft tissue infections, skin flap ischemia, suture dehiscence, and keloid scar formation. Hematomas, seromas and ischemia of the flaps appear immediately after surgery, keloid scars form later, on average during the first year.
Other treatments
The external defect can be reduced using curettage, dermabrasion and laser therapy. The methods are more effective in early childhood, since nevus cells in a child are located in the upper layers of the skin [21][22]. After the procedures, these cells remain in the dermis and over time the pigmentation partially returns. In some cases, melanoma develops in such areas, but the relationship with the treatment has not been proven [23][24][25][26][27].
Contraindications for these procedures are individual. As a rule, these include local disorders: ulceration, cracking, peeling, nodules, tissue immobility and bleeding.
Medical examinations after surgery
Regardless of the treatment performed, patients with large congenital nevi need to undergo a medical and dermatological examination once a year. It is also necessary to palpate the nevus and scars that arise after its removal. If nodules or other suspicious lumps are detected, a histological examination, i.e., examination of tissue samples, is indicated.
Methods for treating blue nevus
Modern medicine offers several effective ways to remove skin tumors:
- Laser surgery involves removing pathological tissue with a high-precision laser beam. The technology allows you to get rid of the tumor in a few minutes. It is important that microsurgery can be performed on hard-to-reach areas of the skin. By adjusting the frequency and depth of the pulses, the laser removes only abnormal tissue without damaging healthy skin.
- Surgical excision is not so popular, because it leaves scars on the skin. The scalpel captures not only the nevus itself, but also the surrounding tissue. This is necessary to prevent relapse. As a result, a large wound takes a long time to heal and requires long-term rehabilitation.
- Electrocoagulation involves the destruction of blue neoplasm cells by electric current. The method is quite painful.
- Freezing tissue with liquid nitrogen is an undesirable procedure when there is a risk of cancer. After all, it is difficult to act accurately with this technology. Rehabilitation after the procedure may take several weeks, as not only pathological tissues die, but also surrounding healthy tissues.
Treatment of blue nevus
As a rule, doctors choose a wait-and-see approach. Patients only need to visit a dermatologist or oncologist regularly for examination. Removal of a blue nevus is necessary only if localization is unsuccessful, causing permanent injury to the formation, and if a number of alarming signs appear:
- a significant increase in its value;
- color change;
- blurred contours;
- the appearance of itching or pain.
To remove a blue nevus use:
- electrocoagulation
- cryodestruction;
- laser;
- radio wave method;
- traditional surgical excision (the nevus is removed along with 5–8 mm of intact skin surrounding it and subcutaneous fat).
Blue nevus: laser removal
In Kharkov, you can sign up for laser removal of a blue nevus at the Lasersvit medical center for diagnosing moles. The clinic diagnoses, monitors and treats various skin pathologies in adults and children. We use modern laser equipment, so we guarantee our patients high results.
Laser treatment of moles, nevi, and other skin tumors is carried out painlessly, bloodlessly, and quickly. Since the laser beam disinfects the wound, there is no risk of infection, and the rehabilitation period is short. The blue nevus disappears without a trace. Look at the photos of our patients before and after surgery to see for yourself.
We employ the best specialists in the region and even in Ukraine, so the treatment takes place without complications. This is confirmed by numerous grateful reviews from our patients. You can learn more about melanocytic neoplasms, risks and treatments by consulting with a qualified dermatologist. Make an appointment at a time convenient for you.
Removal methods and common cases
To remove a nevus, several traditional and innovative methods are used, the decision on which one to choose is made by a dermatologist based on studying the diagnostic results and the general condition of the patient’s body:
Surgical removal of pigmented nevus is widespread. This reliable, repeatedly tested method is optimal for eliminating large-scale formations, “hanging” and other dangerous moles. Disadvantages are a long healing period and a high probability of scar formation, so the surgical procedure is used more often on areas of the body that are permanently covered by clothing;- Today, the cost of laser removal of a nevus on the eyelid, where the skin is especially thin and delicate, has become quite affordable. This method is also effective in most other situations, but the disadvantage is the burning of tissue, which does not allow for histological analysis;
- Cryodestruction is used only to remove flat moles that have captured only the upper layers of the epidermis. In other situations, this technique often leads to relapse and malignancy;
- removal of intradermal nevus of the scalp is performed mainly using advanced techniques - radioknife or laser, although other methods can be used depending on specific indications;
- Almost any method of removing Jadassohn's nevus (sebaceous nevus) is acceptable - surgical scalpel, electrocoagulation, laser, etc. The choice depends on the location and size of the pathological focus;
- Experts often come to the conclusion that there is a danger of a melanoform mole degenerating into a malignant tumor. The price for removing a melanoform nevus in Moscow depends on the chosen technique (any of the currently used ones can be used), the volume of work and its complexity, but it always remains profitable for clients of the MedBioSpectrum clinic.
According to our experts, the best solution in most cases is the removal of pigmented and other nevi with Surgitron. Radio wave technology has a minimum of contraindications, is atraumatic, and ensures rapid tissue healing.
You can get answers to questions, additional information and make an appointment at the MedBioSpectrum MC quickly and easily - right now dial our contact phone number in Moscow or Ramenskoye.