What are nevi
They are a formation consisting of melanocytes. The surface of the mole is smooth and dark in color. There are up to 40 such formations on the body of the average person. Some moles appear on the baby's body immediately after birth. Others are formed during growing up. Nevi can change their appearance and color. Most changes occur during adolescence during puberty. Also, degeneration in a nevus can begin when a person is exposed to direct sunlight for a long time. Ultraviolet radiation in large quantities has a negative effect on the skin. According to statistics, the more time a person spends in the sun, the more moles there are on his body.
The changes concern not only color, but also appearance. An ordinary mole can become flabby and soft, or, on the contrary, develop into a dense and colorless formation. There are a large number of different types of nevi. The main danger of such formations, when exposed to certain factors, is that they can degenerate into malignant ones. Particularly dangerous are complex moles, as well as large formations. They must be constantly monitored by the attending physician in order to prevent a dangerous transformation.
Types of nevi
There are moles on every person's body. Most often they do not pose any danger. If the quantity exceeds 50 pieces, it is advisable to visit a doctor. Such patients are at risk for developing melanoma. Particularly alarming should be asymmetrical formations with an uneven surface, which have a non-standard color, more than 6 mm in diameter, and began to form on the body already in adulthood.
Congenital
This category includes formations with which a person is immediately born. Congenital nevi vary in shape, color and size. In some cases, the mole may occupy a large part of the child's body. Such neoplasms are cause for concern as they often degenerate into cancerous tumors.
Regular
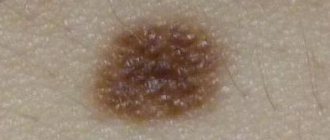
The category of common moles consists of formations that have a symmetrical shape, uniform color and smooth surface. Most often the color is brown or pinkish. There are no foreign inclusions on the surface. Also, such moles can have a dome shape.
Atypical
Moles with non-standard size and appearance. There are few of them on the body, several times less than ordinary moles. The main danger of such neoplasms is that under certain factors they can degenerate into melanoma. Another feature of such formations is that they have an uneven color, uneven edges, and the nevus itself is asymmetrical. For people with atypical moles, it is important to control their number on the body; the more formations, the higher the risk of melanoma. Constant monitoring by the attending physician and completion of the necessary studies is required.
Blue
Neoplasms are divided into two categories: they can appear on the body already in the womb or develop during a person’s lifetime. They got their name due to their bluish color. But this category also includes nevi, the color of which varies from light gray to black. Most often, formations characteristic of the skin of Mongoloids; in other races they develop in extreme cases.
Miescher's nevi
Formations are brown or flesh-colored. The most common place for moles to appear is in the neck and face. The surface is hard, dome-shaped, but smooth, without foreign inclusions. Hair often grows on the nevus.
Nevi of Unna
In appearance they are similar to the moles from the previous description. Features include their appearance: they resemble raspberries. The color of the new growth is brown.
Meyerson's nevus
It is not difficult to determine the problem around such a mole, a rash with red papules begins to develop and spread. In some patients, eczema in the area is not registered. Another feature of Meyerson nevi predominantly develops in men over the age of 30 years. Women are much less susceptible to this problem.
Nevi halo
They got their name due to the atmospheric phenomenon of the same name. A pale whitish ring begins to appear and develop around the mole. Such education does not last until the end of life, even if nothing is done with it. First the ring changes its color to pink, and then disappears. In some cases, new haloes may appear around the tumor throughout the patient's life.
Spitz nevi
Moles are slightly raised above the skin and have a dome shape. The formation itself is pinkish in color; it is acquired and appears on the skin of patients at a young age. Color may be different. The surface of the nevus is often damaged and begins to bleed. As a result, doctors often confuse such moles with malignant ones, referring the patient for histological examination.
Reed's nevi
The color of the formations varies; they can be black or dark brown (closer to a black tint). Mostly develop in women. The peculiarity of the neoplasm is that it increases in size very quickly, which is why it causes concern among doctors. In fact, such moles are mostly harmless and rarely develop into cancer.
Agminated
They are several moles at once, which are concentrated on a small area of the skin. The peculiarity of formation is that all nevi are not the same. Some may be more, some may be less. Also, among flat formations, dome-shaped ones, etc., may appear.
Only the main types of moles are listed above. In fact, there are a huge number of such neoplasms on the skin. To determine what type of mole a particular mole on the body of a patient seeking medical help belongs to, doctors perform dermatoscopy.
Benign pigmented skin neoplasms (moles)
Nevus ( noncellular nevus , pigmented nevus , nevoid tumor , birthmark ) is a pigmented (colored) formation on the skin, which includes nevus (pigment) cells. Nevi are benign neoplasms; most researchers associate their occurrence with the migration in the embryonic period of the precursors of pigment cells (melanoblasts) from the neuroectodermal tube to the basal layer of the epidermis.
The nevus is of particular interest due to the fact that in place of a pre-existing congenital or acquired benign nevus, such a formidable malignant neoplasm as melanoma .
Almost all people have various congenital and acquired nevoid neoplasms. More than 90% of the population has pigmented skin tumors. The average number of nevi in each person is 20, ranging from 3 to 100, and their number usually increases with age. Not all nevi can potentially degenerate into melanoma, so they are usually divided into melanoma-hazardous and melanoma-non-hazardous.
Melanoma-dangerous nevi are much less common (about 10%) than melanoma-non-dangerous nevi. These nevi do not differ in the age of patients, localization of lesions and other clinical and anatomical data. It is important to consider that it is impossible to carry out differential diagnosis based on the degree of pigmentation of the lesion. Various injuries - mechanical, chemical, radiation, both acute and repeated - can be factors that provoke the transformation of some types of nevi into melanoma, primarily borderline or other melanoma-hazardous ones. In this regard, a biopsy of a suspicious skin element is strictly contraindicated, as well as its cosmetic treatment using directly traumatic methods (partial removal, electrocoagulation, cryotherapy, exposure to chemical and other agents). The percentage of melanoma patients who have clear indications of trauma preceding the development of the tumor (after incomplete cosmetic removal of a pigmented nevus, accidental trauma) varies from 20 to 78%. A biopsy or incomplete removal of the lesion in order to distinguish a melanoma-dangerous nevus from melanoma or other skin lesions is strictly unacceptable.
General principles of treatment of pigmented neoplasms
Any pigmented skin growths require special attention. Greater caution should be shown to nevi localized in traumatic areas of the skin, as well as to previously injured nevi that are rapidly growing or rapidly changing their pigmentation.
Therapeutic tactics for pigmented nevi boil down, first of all, to the categorical refusal of any traumatic treatment methods: electrocoagulation, cryodestruction and the use of various cauterizing solutions.
Treatment of pigmented neoplasms is radical surgical excision of the lesion within intact skin. The use of modern non-traumatic suture materials and the rules of aesthetic surgery makes it possible to achieve barely noticeable postoperative scars. Surgical treatment (excision along the edge of the formation), as well as various cosmetic manipulations (cryodestruction, chemodestruction) of melanoma-free neoplasms do not carry the risk of malignant transformation of these formations.
A completely different tactic is followed for melanoma-dangerous nevi. If a melanoma-hazardous formation is suspected, the patient should be immediately sent to an oncologist! The tactics and technique of surgical intervention are determined by the location and size of the melanoma-dangerous pigmented nevus. The best limits for excision on the trunk and limbs, taking into account, on the one hand, the clear limitation of “quiet” nevi and, on the other hand, cosmetic considerations, is considered to be a distance of 0.5 cm in all directions from the borders of the nevus; this is quite sufficient for the prevention of melanoma. The nevus is excised with surrounding incisions along with the surrounding skin and the surface layer of tissue; the tissue is sutured with a cosmetic suture using non-traumatic suture material, which allows one to achieve good cosmetic results. On the face, neck, auricle, fingers and nail bed, for anatomical and cosmetic reasons, more economical excision of melanoma-dangerous nevi is allowed, but not less than 0.1-0.2 cm from their borders. On the face and neck, sutures are applied with a very thin thread, which allows for maximum cosmetic effect. In all cases of surgical excision of a pigmented nevus without exception, histological confirmation of the diagnosis is necessary - i.e. the excised area is necessarily sent for microscopic examination; if the result is atypical cells (melanoma), the patient is referred to an oncologist.
Patients who refuse radical surgical treatment, as well as in the case of its impossibility due to difficult anatomical localization, should carefully protect their tumor, exclude its injury, solar radiation and be monitored by an oncologist.
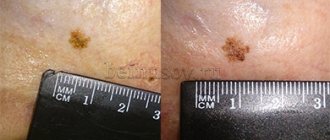
Borderline pigmented nevus
A borderline pigmented nevus is a flat dark brown or black nodule up to 1 cm in diameter with a smooth, dry surface, develops at the border of the epidermis and dermis, and is characterized by increased activity of pigment cells (melanocytes). Sometimes a border nevus looks like a spot of round or irregular shape with smooth wavy edges. Borderline nevus does not have a favorite location. It can be located on the skin of the face, neck, and torso. Pigmented nevi on the skin of the palms, soles, and genitals are almost always borderline. Borderline nevus is most often congenital, but can appear in the first years of life or even after puberty. An important differential diagnostic sign of a borderline pigmented nevus is the complete absence of hair on it.
Pigmented border nevus must be distinguished from cavernous hemangiomas, which are characterized by a softer consistency of the node, from seborrheic (“senile”) keratoma, which, as a rule, has a less smooth, “rough”, greasy surface. In the differential diagnosis between borderline pigmented nevus and early melanoma, anamnesis plays an important role. Most patients with melanoma indicate that their tumor developed in place of a pigmented nevus that existed for a long time or even from birth, which did not cause any inconvenience. The nevus grows slowly according to body weight. During puberty, patients may notice an acceleration in nevus growth - a consequence of hormonal changes and an increase in the level of metabolic processes, including pigmentation. Mechanical trauma is the predominant factor accompanying the malignancy of previously “quiet” nevi.
The following borderline nevi are especially dangerous: systematically injured, located on the sole, nail bed, or in the perianal area. Timely removal of nevi in these localizations is a reliable prevention of melanoma. Excessive insolation, thermal or balneological treatment of concomitant chronic diseases also play a negative role in the development of melanoma. Acceleration of nevus growth after injury or active insolation, inflammatory changes, discoloration, the appearance of itching, weeping, and induration should be alarming.
Blue or blue nevus
Blue or light blue nevus (Jadassohn-Tiche nevus) is a dark blue or bluish node, sharply demarcated from the surrounding skin, round in outline, densely elastic consistency with a smooth, hairless surface. The blue color is due to massive accumulations of melanin in the deep layers of the dermis. The size of the node, as a rule, does not exceed 0.5 cm. Blue nevus is most often located on the face, limbs, and buttocks. In most cases, blue nevus is a solitary formation. Blue nevus occurs in all age groups, most often in middle-aged women . Clinically, a blue nevus is difficult to distinguish from a pigmented borderline nevus. However, clinical features such as large demarcation and infiltration, blue or blue color, appearance at a later age and hemispherical shape allow for a differential diagnosis. With a deeper location in the skin, a blue nevus sometimes has to be differentiated from a dermatofibroma. Symptoms such as less infiltration, color and usually a solitary lesion help to distinguish it. The development of melanoma at the site of a blue nevus is rare, but this nevus is classified as melanoma-dangerous .
Nevus Ota
Nevus of Ota, or oculodermal melanocytosis, is a large, usually unilateral pigmented nevus on the face in the area of innervation of the I and II branches of the trigeminal nerve (the area of the forehead, cheeks and nose). Clinically, dark brown pigmentation is noted in various parts of the eye: conjunctiva, sclera, iris. At the same time, a massive pigmented nevus (or nevi merging with each other) is detected on the cheek, upper jaw and zygomatic region of the same side, black and bluish in color. All this creates the impression of “dirty skin” on the affected side of the face. In rare cases, the red border of the lips and the mucous membranes of the soft palate, pharynx, larynx and nose are affected. Women get sick more often. Nevus of Ota is congenital, but can occur in early childhood or even during puberty. It usually grows slowly. Apart from cosmetic inconveniences, it does not cause any disorders, including visual impairment. There are known cases of melanoma developing in its place. Close to the nevus of Ota and an even rarer variety is considered to be the nevus of Ito, located in the supraclavicular, scapular regions and the deltoid muscle region.
Giant pigmented nevus
A giant pigmented nevus is always congenital, increases in size as the child grows, reaching a large size (from the palm of the hand or more) and sometimes occupies a large part of the torso, neck and other areas. Usually, over a considerable extent, the surface of the nevus is lumpy, warty, with deep cracks in the skin. Areas of hypertrichosis (hair nevus) are common. The color varies from grayish to black and is often heterogeneous in different areas. Malignancy of a giant pigmented nevus occurs in 1.8-10.0% of cases. Treatment tactics for suspected pigmented borderline and blue nevi, especially if they are located on accessible insolation and frequently injured areas of the skin, boil down to the categorical refusal of any traumatic treatment methods: electrocoagulation, cryotherapy, the use of various cauterizing solutions and incomplete surgical excision. If necessary, economical surgical excision of the lesion with the surrounding skin is performed at a distance of 0.5 cm in all directions from the borders of the nevus along with subcutaneous fatty tissue; this is quite enough to prevent melanoma. On the face, neck, auricle, fingers, due to anatomical features, a more economical excision of melanoma-dangerous nevi is permissible with a deviation of 0.2-0.3 cm from its borders. For giant nevi, which cause great cosmetic inconvenience to patients, step-by-step excision is used, followed by skin plastic surgery .
Dubreuil's melanosis
Dubreuil's melanosis is a nevoid formation, the connection of which with melanoma is indisputable. Dubreuil's melanosis usually begins as a small brownish pigmented spot that slowly spreads around the periphery. A clinically mature lesion has blurred boundaries and an uneven surface of dark brown and sometimes black color, more saturated than the color of pigmented nevi. Within the formed focus there are areas of different shades (brown, gray, black, bluish). The skin pattern over the lesion remains unchanged and becomes rougher. Elements resembling a senile wart may appear. Sometimes atrophy, hyperkeratosis, and flat surface papillomatosis develop. Characterized by increased pigmentation along the periphery of the lesion. Inflammatory phenomena are extremely rare. In most patients, Dubreuil's melanosis manifests itself in one focus. The most common location is open areas of the skin, especially the face (cheeks, nasolabial folds, nose, forehead), less often the neck and scalp. Dubreuil's melanosis mainly affects older people, which allows it to be classified as a senile dermatoses. The clinical picture of limited precancerous Dubreuil's melanosis, especially in the stage of a formed lesion, in most cases is so characteristic that it does not cause great diagnostic difficulties.
Differential diagnosis must be made with large seborrheic (senile) keratoma, pigmented basal cell carcinoma, and some forms of nevi. However, all these nosological forms are characterized by clearly demarcated lesions. With basal cell carcinoma, a raised ridge with “pearls” is visible (especially through a magnifying glass); the central part of the tumor is often ulcerated. The surface of a seborrheic keratoma is more lumpy and often “greasy” to the touch. A clinical symptom such as uneven hyperpigmentation, as well as medical history - onset of the disease in old age and very slow progression of a single lesion - are very helpful in diagnosing Dubreuil's melanosis.
The causes of malignancy of Dubreuil's melanosis have not been established; trauma and insolation are considered to be the impetus for the onset of invasive tumor growth . Dubreuil's melanosis is a more pre-melanoma skin lesion than borderline pigmented nevus, not to mention other melanoma-dangerous nevi. Therefore, Dubreuil’s melanosis is considered not so much melanoma-dangerous as directly pre-melanoma and even an absolute precancer of the skin .
The treatment strategy for Dubreuil's melanosis differs significantly from that for melanoma-dangerous nevi. First of all, it is unacceptable to leave patients without active treatment , which is possible with Ott’s nevus and other melanoma-dangerous nevi after warning patients about the danger of injury. Another difference is that wide surgical excision of Dubreuil's melanosis , given its predominant location on the face, is associated with serious technical and cosmetic difficulties, especially with large lesions . Sometimes excision of large lesions on the body is completed with plastic surgery using displaced flaps. The method of choice for Dubreuil's melanosis on the trunk and limbs is excision of the lesion, 0.5 cm from its edges.
Fibroepithelial nevus
Fibroepithelial nevus belongs to the group of melanoma-NON-dangerous nevi and nevoid skin lesions . Fibroepithelial nevus, along with pigmented intradermal nevus, is the most common nevoid formation on human skin and the most common reason for visiting a surgeon. Fibroepithelial nevus often first appears during various periods of intrauterine life, sometimes existing from birth. Its growth is usually very slow. Localization can be very different, but mainly on the face and torso. The number of formations varies from one to several dozen. Histologically, fibroepithelial nevus has the structure of a soft fibroma.
Clinically, a fibroepithelial nevus is a hemispherical, painless formation rising above the skin level with a soft or soft-elastic consistency ranging from a few millimeters in diameter to the size of a bean and, rarely, larger. Color varies from normal skin or pinkish-red (usually with a slight bluish tint) to bluish-violet and dark brown. With the latter or close to it coloring, the greatest difficulties arise in differential diagnosis with borderline pigmented and blue nevus. The shape of a fibroepithelial nevus is usually regular, round, and the surface is smooth, although less smooth than that of a borderline pigmented nevus. The surface of the nevus is often penetrated by single vellus or bristly hairs or even a coarse tuft of hair, especially in women (fibroepithelial pilaris nevus). With a pronounced vascular component in the form of a telangiectatic mesh on the surface, they speak of angiofibroepithelial nevus, which can also be hairy.
In most patients, there is no inflammation around the fibroepithelial nevus. Sometimes after an injury the nevus becomes inflamed (when shaving the face, after a blow). In these cases, an inflammatory rim develops around the circumference. In typical cases, diagnosing a non-inflammatory fibroepithelial nevus is not difficult. Differences from borderline pigmented and blue nevi: color (even with pigmented fibroepithelial nevi, the color is less saturated), shape, multiplicity, frequent presence of hair. In its clinical picture, an inflamed fibroepithelial nevus differs sharply from the picture observed during malignancy of a melanoma-dangerous nevus.
Papillomatous nevus
Papillomatous nevus has an uneven, bumpy surface, often localized on the scalp, but can also occur on any other part of the skin. The sizes are often large, up to several centimeters, the outlines are irregular, the color varies from the color of normal skin to brownish, less often - dark brown or even black. Like fibroepithelial nevus, papillomatous nevus is often riddled with hair. As a result of injury, the papillomatous nevus becomes inflamed. The location of the papillomatous nevus on the face and other open areas of the skin causes patients to persistently desire to get rid of the formation, which can be subjected to cosmetic treatment.
Verrucous nevus
Verrucous nevus is a clinical type of papillomatous nevus. Its surface is even more lumpy, in pronounced cases it has the appearance of a “head of cabbage”, penetrated by deep folds and cracks. It protrudes significantly above the surface of the skin and is usually more pigmented (pigmented, or pigmented verrucous nevus). Like papillomatous nevus of the extremities, most often there is a single focus. Clinical recognition of verrucous nevus does not present any particular difficulties. Sometimes, especially if it is small, a verrucous nevus can be mistaken for a giant common wart. Correct recognition is helped by anamnestic data (exists from birth or early childhood, grows very slowly), frequent presence of hair on the surface; usually the lesion is single. The treatment and tactical approach is similar to papillomatous nevus.
Halo nevus (Setton's nevus)
Halo-nevus is clinically a reddish-brown nodule, slightly raised above the skin level, 4-5 mm in diameter, round or oval, surrounded by a rim of depigmented skin. The width of the depigmented area is 2-3 times greater than the diameter of the hyperpigmented nodule. Halo nevus is often multiple, predominantly localized on the torso and arms, less often on the face. Often, Halo nevus undergoes spontaneous regression. The clinical picture of Halo-nevus is typical and does not cause differential diagnostic difficulties. The development of melanoma at the site of the Halo-nevus, even after injury, is not observed. It has been noted that Halo nevus sometimes occurs in malignant tumors of internal organs and melanoma.
"Mongolian Spot"
“Mongolian spot” is an irregularly shaped rounded skin lesion, colored bluish or brownish, up to 5-6 mm in diameter, located exclusively in the lumbosacral region. The “Mongolian spot” is almost always a congenital formation; in most patients it disappears without a trace in childhood. The development of melanoma at the site of the “Mongolian spot” is not observed and does not require treatment.
Intradermal nevus
Intradermal nevus, or common birthmark, occurs in almost all people. Birthmarks are located in the skin and mucous membranes. Most often, these nevi are congenital; the pigmentation is usually brown. For the vast majority of people, birthmarks do not cause cosmetic discomfort.
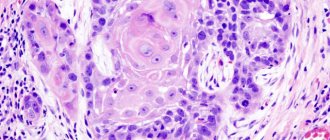
Dysplastic nevus
Dysplastic nevus is an acquired pigment formation, histologically represented by a random proliferation of polymorphic atypical pigment cells (melanocytes). It occurs on clear skin or as a component of a complex nevus. Dysplastic nevus has characteristic clinical and histological features that distinguish it from acquired noncellular nevi. It is considered a precursor to superficial spreading melanoma and is considered a risk factor for melanoma.
Dysplastic nevus are pigmented spots of irregular shape and with unclear boundaries, slightly raised above the skin level, their color varies from reddish-brown to dark brown on a pink background. Dysplastic nevi first attracted attention for their unusual appearance and increased frequency in some families (they are inherited). As a rule, they are larger than ordinary birthmarks, reaching 5–12 mm in diameter; the localization is also different: dysplastic nevi, although they can occur anywhere, are more often found in areas usually covered by clothing (on the buttocks, chest), or on the scalp. Most people have an average of 10 ordinary moles, while dysplastic nevi can have more than 100. Ordinary nevi usually appear during puberty, while dysplastic nevi continue to appear even after 35 years.
Comparative characteristics of dysplastic nevus and acquired noncellular nevus
| Sign | Dysplastic nevus | Acquired noncellular nevus |
| Color | Heterogeneous - various combinations of light brown, brown, black, red and pink; dysplastic nevi can differ significantly from each other | Uniform - light brown or brown |
| Form | Incorrect; fuzzy, blurred boundaries; peripheral areas are at skin level | Regular, round or oval; boundaries are clear; the formation is either at the level of the skin or evenly raised above it |
| Dimensions | Usually > 6 mm in diameter, often > 10 mm; occasionally < 6 mm | Typically < 6 mm in diameter |
| Quantity | Often multiple (> 100), but single lesions possible | On average, an adult has from 10 to 40 nevi; approximately 15% do not have them at all |
| Localization | Open areas of the body, most often the back; found on the scalp, mammary glands and buttocks | Typically exposed areas of the body above the waist; scalp, mammary glands and buttocks - extremely rare localization |
Vascular nevus
Vascular nevus (naevus flammeus, port-wine stain) is an anomaly of the capillaries of the dermis, manifests itself in the form of a spot from light pink to red-brown. Vascular nevus, located in the center of the face or back of the head, is not combined with other developmental defects and usually fades with age. With an asymmetrical, unilateral localization (on the face or limbs), a vascular nevus is usually one of the manifestations of Sturge-Weber syndrome or Klippel-Trenaunay syndrome. In this case, with age, the nevus usually darkens, and its surface in some places becomes bumpy and rises above the skin level.
Capillary hemangioma
Capillary hemangioma or strawberry nevus is the most common congenital vascular tumor. It begins as one or more pale pink papules that grow rapidly, become lobulated, and range in color from bright red to dark blue. Capillary hemangiomas appear at 3-5 weeks of life; 70% of them disappear spontaneously by the age of 7 and do not require treatment. Treatment. If the location and rapid growth of the tumor lead to visual or respiratory problems, resort to the injection of corticosteroids into the lesion, cryodestruction, laser therapy or surgical excision.
Papillomatous nevus
There are a large number of neoplasms found on the human body. Not all of them are moles. Thus, warts, condylomas, papillomas and other formations may appear. When making a final diagnosis, the whole difficulty lies in the fact that the listed types of neoplasms are often no different in appearance from ordinary nevi. The most problematic is considered to be papillomatous nevus. In appearance, it is no different from ordinary papilloma caused by HPV. But when conducting research, it turns out that this is a bumpy mole of a convex type. The mole is benign, there is no risk of degeneration into cancer. The surface has a flesh-colored, brownish or light brown tint. Dark moles of this type are extremely rare.
A characteristic feature of such moles is the presence of hair on the surface. They mainly appear on the head or neck; they can develop in other parts of the body, but in very extreme cases.
The appearance is not tied to a specific age period. They develop in both teenagers and old people. The mole grows over time, sometimes it increases in size so much that it begins to cause discomfort to the wearer. If the nevus is located on the head, it can be easily damaged when combing the hair. This leads to the onset of inflammatory processes that affect nearby tissues.
The nevus is harmless; its removal is generally carried out only for cosmetic purposes. The greatest discomfort for people is caused by moles on the face, which are visible to everyone around them. Before deciding to undergo a tumor excision procedure, it is important to consult a dermatologist. Only after all the studies have been carried out will the specific type of nevus be established, and the likelihood of the problem degenerating will be assessed. It is almost impossible to independently determine what exactly appears on your body.
Indications for removal may also be permanent damage to the surface of the nevus. Most often, several methods are used to combat education:
- Laser treatment of the area;
- Freezing and subsequent destruction;
- Radio wave exposure;
- Using electric current;
- Surgical intervention.
If the formation appears on the face, laser therapy is most often chosen.
Methods for removing pigmented nevi
- Small nevi are removed using a laser. Local anesthesia is used here and many small nevi can be removed at once in one visit. A crust appears at the site of removal, which will disappear in seven days. The marks are practically invisible, which is why the laser method is used to remove facial moles.
- For large nevi, surgical excision is used. The operation is performed under local or general anesthesia with suturing.
The decision on the treatment method is made as a result of examining the nevus. In some cases, consultation with an oncologist is required. When surgical excision is used, the tumor is sent for histology to determine whether it is melanoma.
You should never remove moles and birthmarks yourself. This is fraught with infection and other troubles.
Conventionally, pigmented nevi can be divided into four categories according to their size:
- small (up to 1.5 cm)
- medium (up to 10 cm)
- large (up to 20 cm)
- giant (more than 20 cm)
Multiple pigmented nevi are quite rare (5%). This nevus consists of a large lesion and small pigment spots and affects the lower body, limbs, back and chest.
Intradermal nevus
A type of ordinary nevi that have a dome-shaped shape. Such moles rarely appear in childhood, but they are extremely common in the adult population. Up to ten such formations can appear on the body at the same time. Such neoplasms got their name due to the fact that they are located under the upper layer of the epidermis. Often such moles are difficult to notice; they hardly stand out above the surface of the body, and their shade is close to the surrounding tissues.
Nevus can appear in almost any area. Favorite places for neoplasms are the upper part of the arms, eyelids, neck, face, etc. The maximum size of moles is up to 1 centimeter. When they appear in childhood, nevi are practically invisible, but with age they begin to darken and often acquire a convex shape. If the mole persists, then after 70 years it will gradually begin to discolor.
There are several reasons why intradermal nevi can form on the human body:
- Hereditary factors
. If the baby’s parents have more than 50 ordinary moles on their body, then the child’s nevi will also be multiple in nature. - Exposure to sunlight
. Ultraviolet radiation negatively affects the skin, causing damage. Moles often appear in place. People with too light skin are at risk. - Decreased immunity
. Most often, nevi begin to form against the background of reduced immunity, including after taking drugs that suppress the immune system.
Even ordinary moles that have a symmetrical appearance and do not increase in size are important to constantly monitor. It is better to have a checkup with a dermatologist at least once a year, this way you will be able to identify the problem at an early stage of its occurrence. It is worth planning a visit to a specialist outside of the schedule if the mole begins to grow, changes its shape, acquires a different shade, or begins to bleed.
A dermatologist may prescribe a procedure for excision of a mole if it causes cosmetic discomfort to the wearer, if there is a risk of the neoplasm degenerating into melanoma, if the surface of the nevus is constantly damaged during the day.
Dysplastic nevus syndrome
Unfortunately, there is a syndrome that in Russian literature is often called nevus dysplastic syndrome (in foreign literature - FAMMM).
This disease has 2 diagnostic criteria
- the number of dysplastic nevi on the skin is more than 50
- melanoma in relatives
This disease may be associated with a mutation in the CDKN2A gene, which also increases the risk of developing pancreatic cancer
With this syndrome, the risk of developing melanoma, according to different authors, varies from 56 to 100%. The disease requires regular (once every few months) monitoring by an oncologist.
Epidermal nevus
As the name implies, this category includes moles that are formed from the upper cells of the epidermis. Mostly, neoplasms appear on the child’s body after birth; the vast majority of such nevi also appear in the first year of the baby’s life. A distinctive feature of the neoplasm is that it remains unchanged in shape and size throughout a person’s life.
Epidermal nevi are divided into several types depending on the cells that make up them. The most unpredictable are considered to be formations that include not only keratinocytes, but also sweat gland cells. The formations have a yellow-orange tint; in 25% of cases they degenerate into malignant tumors.
Differential diagnosis
To make an accurate diagnosis, a dermatologist must conduct a series of tests, since the symptoms of linear moles are similar to those of other skin diseases.
At issue are:
- warty neurodermatitis
- characterized by lycosis and itching; - lichen planus papillary
- characterized by itching and its occurrence at a later age, determined by the presence of typical lesions of lichen planus in other places and histological examination; - lichen striata - characterized by inflammatory papular rashes and spontaneous resolution within a few months.
Non-pigmented moles
Most species are characterized by a color ranging from light pink to black. There are a few exceptions to the rule. So, sometimes a nevus may not have pigment. Such moles are easy to identify; they appear as a whitish or lightish spot with unclear boundaries and an irregular shape. Moles without pigment can only appear on the body of Europeans.
Moles without pigment are characterized by a small size of up to 2 centimeters. Basically, only the cosmetic side of the issue becomes an indication for removal. If a person often sunbathes, the nevus remains light in color and, as a result, stands out on the skin and attracts attention.
Out of sight, out of sight. How to get rid of moles
Not an easy question. Many factors influence the ability to remove tumors. Unfortunately, no pills have yet been invented that will relieve you of annoying or dangerous moles.
Yes, treatment of small nevi usually does not cause problems.
Successful removal depends on:
- Doctor's qualifications
- Mole size
- Nevus locations
The first option is surgery. The doctor cuts off the mole, some adjacent skin, and then stitches the wound. After removal, the nevus heals quite quickly, but a noticeable mark remains.
Whether this is good is up to you to decide.
What about laser surgery?
Yes, modern technologies do offer new treatments, but they do not work miracles, as some people believe. Some skin diseases are treated with lasers. But not all nevi.
The laser beam vaporizes the outer layer of skin and cells of the mole. The deeper it is rooted, the more difficult it is to destroy it completely - sometimes the surface layer is burned out, but the base remains intact. Then the nevus grows back.
The operation has to be repeated again and again, and there is no guarantee of results. So the surgical procedure is sometimes more reliable than laser surgery.
However, in some situations, a high-tech procedure accomplishes the task. Removes small nevi. Working with large tumors is much more difficult.
We recommend choosing laser nevus removal only after consulting a dermatologist and checking the tumor.
Another important point is the choice of doctor. Many doctors have accumulated vast experience in removing small moles. Everyone has them. Therefore, doctors work with them very often and know well how to quickly remove nevi.
But what about large moles?
They are not common and therefore it is difficult to find a doctor who regularly operates on them. Read reviews about nevus removal on the websites of different clinics. This is useful. You will learn what operations the doctors of these medical institutions performed and the patients’ impressions of their work.
Gather more information.
When you see your dermatologist, ask about available methods for removing moles. Perhaps in your case, surgery and laser therapy are not the best options. Harmless nevi do not need to be removed at all.
Many medical institutions remove moles. But where to go? We would like to recommend one of these clinics.
Borderline nevus
The formations got their name due to the fact that they often develop into malignant formations. It is important to constantly monitor such moles and contact a dermatologist if any changes are detected.
Such moles are hidden under the stratum corneum of the skin; they have a uniform brown color and clear boundaries. The following factors should cause concern in the patient and provoke a visit to a dermatologist:
- the mole begins to increase in size;
- changes its color, becomes darker or lighter;
- pigment spots of various types began to appear around the adjacent area;
- the mole has become dense, standing out above the surface of the skin;
- Soreness appeared in the mole, the surface was very itchy.
Treatment options for intradermal mole
Intradermal nevi have several treatment options:
- laser therapy (nevus is treated with a laser);
- cryodestruction (the formation is frozen with liquid nitrogen);
- surgical method (the mole is removed with a scalpel);
- electrocoagulation (the nevus is cauterized with a special electric knife);
- radiosurgery (a mole is removed using a radio knife).
Before prescribing treatment, the doctor is guided by the size of the mole, its appearance, color, location, as well as the likelihood of it becoming malignant.
If there is even the slightest risk of the nevus turning into melanoma, the doctor will definitely prescribe removal of the mole with a scalpel. During this procedure, tissue located near the tumor is also removed to prevent tumor development.
Many doctors consider laser surgery to be the most effective treatment for intradermal nevi. It is especially good for removing large birthmarks that are more than 3 cm in diameter, as well as skin melanoma.
Laser surgery has a number of advantages over other methods of treating nevi:
- There is no bleeding during removal, because all small vessels are immediately cauterized;
- healthy tissues and cells are not affected, which means they are not injured;
- there is no need for postoperative sutures;
- the rehabilitation period after the operation is minimal;
- There are practically no scars left.
What to do with huge nevi
The overwhelming majority of nevi are small formations on the skin with a diameter of several millimeters, which are practically invisible to the naked eye. Exceptions are formations that exceed 20 centimeters in diameter. They are classified as huge. The mole can cover most of the arm, leg, back, etc. Such moles can appear on the body of representatives of any race. They develop in almost 2% of the population of our planet. The main danger of large nevi is that they often degenerate into malignant ones. Formations that appear in the area of the spinal column are considered extremely unstable. Moles that continue to rapidly increase in size and also change their color should cause concern.
The most unpleasant huge nevi on the body of newborn children. As the child grows over time, it seems to parents that the mole is decreasing in size, but in fact it continues to grow, almost not keeping up with the whole body.
In 30% of cases, such nevi become melanoma. They should be under the supervision of a doctor. Rebirth can occur at absolutely any age. Removal of giant nevi is indicated. The most commonly used method is surgical excision. If the mole is located in a hard-to-reach place, the patient may be offered alternative treatment methods. Removal is also possible using laser therapy.
How are nevi treated in the Rassvet blade?
The doctor will examine the patient's skin completely to eliminate the risk of missing melanoma or other skin cancer. Suspicious formations are further studied using a device that allows you to examine the skin with 10 times magnification - a dermatoscope. The patient's chart describes nevi that require observation. The doctor will suggest surgical removal of suspicious nevi, followed by histological examination of the removed material (sent to an expert laboratory). Removal of nevi for aesthetic reasons can be performed at the request of the patient.
Recommendations of a dermatologist for patients with nevi:
- avoid excessive ultraviolet irradiation of the skin (tanning, sunbathing, solariums, ultraviolet drying of manicure and pedicure coatings); when staying outdoors for a long time, use a broad-spectrum photoprotective cream with SPF 30 or higher, clothing that covers the skin, a hat and glasses with an ultraviolet filter;
- try not to injure nevi when shaving, combing, changing clothes;
- undergo an annual preventive examination of nevi with a doctor;
- independently examine nevi according to the ABCDE rule;
- if there are a large number of nevi (50-100 or more), especially in combination with the presence of risk factors (sunburn, visits to a solarium, melanoma and skin cancer previously identified or in close relatives, the presence of atypical nevi), undergo a digital skin mapping procedure.
Author:
Kuzmina Tatyana Sergeevna dermatologist, Ph.D.
Nevi on the head
Such formations are most often removed precisely for cosmetic reasons. If a mole is located on the surface of the body, no matter what size it is, it can almost always be hidden under clothing. Nevi on the head cannot be hidden. Some patients believe that a mole emphasizes their individuality, others are sure that such a formation only spoils their beauty. As a result, patients often seek removal of even those nevi that will never become malignant.
Often, not only moles on the head are removed, but also tumors on the neck. The main danger of such moles is that they often rub against the surface of clothing and are eventually damaged, which increases the risk of degeneration. On the head, nevi also appear in the hair area. They are practically invisible to the naked eye and are often felt by the patient during hair washing and other procedures. The main danger of neoplasms is that they can be easily damaged during banal combing of hair. Nevi, which include cells of the sebaceous glands, also often appear on the scalp in the hairline area. They are characterized by the shape of a wart with no hair on the surface, as well as an irregular shape. Human papilloma viruses, as well as hereditary factors, can cause the appearance.
Most moles on the head appear at birth. The formation is examined and research is done to make a final diagnosis. In childhood, neoplasms are rarely removed, since they are not subject to degeneration during this period. It occurs most often during puberty. The removal method is selected depending on the size of the formation. If the nevus is small, you can get rid of it with laser therapy; to combat large formations, surgery will be required.
It is important to remember that at the moment there is no magic pill that could remove all dangerous moles from human skin that can become malignant. It is important to monitor the condition of nevi and pay attention to any changes.
Moles are successfully removed. It all depends on the size, qualifications of the medical specialist, as well as the location of the nevus.
Types of treatment
Pathologically, nevus of Ota is a melanocytic hamartoma that is located at the level of the middle dermis. Therefore, treatment methods must penetrate to this depth9,10.
Highlight:
- Cryotherapy (may cause scarring)
- Surgical excision
- Carbon dioxide
- Argon
- Chemical peeling
- Dermabrasion
- Hydroquinone-based bleaches
- Laser:
- QS ruby (595 nm)
- QS Nd:YAG (1064 nm)
- QS alexandrite (755 nm)
- Picosecond laser