Papillomas on the cervix: causes and treatment
Speaking about the reason for the appearance of papillomas, we are entering one of the most mysterious areas of medical knowledge - the nature of viruses.
These microscopic formations have a non-cellular structure, unlike most organisms living on Earth. They exist exclusively by parasitizing living cells. The papillomavirus we are interested in (HPV or HPV) penetrates skin cells, integrates into chromosomes and changes the tissue growth program. Cells begin to rapidly divide, growing to form papillomas. More than a hundred strains of HPV have already been identified, but not all of them are well studied.
What kind of virus is it and where does it come from?
The human papillomavirus (HPV) lives in the blood, appears on the skin and mucous membranes and is transmitted from these areas by contact - by touch, i.e. it is not an infection transmitted exclusively through sexual contact. Moreover, the human papillomavirus can live in the body for a long time, even from birth, and appear for the first time in the middle of life due to a decrease in immunity.
You cannot associate the first manifestation of the virus with a recent infection - it could have happened a long time ago, although you did not know it.
According to official statistics, the prevalence of HPV is quite high - up to 70%, although doctors in their practice encounter it in 90% of cases. Fortunately, not all types of the virus are oncogenic.
Why do papillomas appear?
There is only one reason for papillomas on the cervix – the entry of a virus into the body. But there are several ways through which he can penetrate. We list them in order of increasing likelihood of infection:
- Sexual contact with an HPV carrier. At the same time, the use of condoms, according to experts, is not able to protect against infection.
- Everyday route: when visiting public institutions (baths, swimming pools, etc.), through the use of hygiene items shared with the carrier.
- A child can become infected during childbirth if the mother has an acute form of the disease.
The immune system of a healthy person is so strong that it is able to overcome the papilloma virus. If immune cells control the virus, external forms of the disease do not develop immediately after infection. However, when the defenses are weakened (severe stress, fatigue, excessive alcohol consumption, smoking), the virus can become more active and cause the formation of papillomas, as well as associated pathologies.
How are papillomas diagnosed?
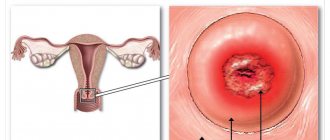
Exophytic papillomas (genital warts) of the cervix are quite simply diagnosed visually during a routine gynecological examination.
To improve visualization, the formations are treated with a 5% acetic acid solution.
As a result, a characteristic whitish-gray color appears and the vascular pattern intensifies.
Also, uneven staining with Lugol's solution is typical for papillomas.
Endophytic condylomas are difficult to distinguish by simple examination.
They can be seen only with the simultaneous presence of genital warts or with significant keratinization.
That is why, if such formations are suspected, the results of cytology and colposcopy become very important.
When making a diagnosis, a differentiation is made between flat condylomas and Naboth cysts (cysts of the cervix formed due to blockage of the gland ducts).
The disease is finally confirmed after histological examination.
Cytological examination (study of cellular structures) is also carried out for simple pointed papillomas on the uterine cervix.
Such tests can exclude cancer.
Molecular biological methods (PCR - polymerase chain reaction) are also used to assess the viral load and determine the type of virus.
Additionally, especially in preparation for surgical removal of papillomas, tests for HIV, syphilis, hepatitis B and C, and other urogenital infections may be prescribed.
The need for the latest tests is also determined by the fact that 90% of episodes of HPV infection are accompanied by the presence of other infections.
Diagnostic and therapeutic procedures are prescribed by a gynecologist, dermatologist, and venereologist.
If necessary, consultations are provided:
- obstetrician-gynecologist, if pathology is detected in a pregnant woman
- urologist, if you suspect the presence of formations in the urethra
- an immunologist if the disease developed against the background of immunodeficiency conditions and/or is characterized by persistent recurrence
Dysplasia and papillomas
If left untreated, highly oncogenic papillomavirus (mainly types 16 and 18) can lead to dysplasia. This is a precancerous condition in which a violation of the structure of the cervical epithelium and the replacement of normal cells with atypical ones are detected. This process is not yet malignant, but over time it can lead to cancer. The time of this transition is individual for each woman and depends on many factors: the strength of the immune system, heredity and others.
According to the observations of practicing doctors, the time for the degeneration of dysplasia into an oncological process varies from 10 to 20 years. If you get rid of the cause of cervical dysplasia - the papilloma virus - as early as possible, this will eliminate the unfavorable prognosis of the disease.
The best way to prevent cancer is regular examinations with a gynecologist and taking a control smear for oncocytology. You should visit a gynecologist every six months. Women who are HPV carriers should especially strictly follow these recommendations.
HPV in women: how to keep your cervix healthy
More than 660 million people in the world are infected with the human papillomavirus. The main danger of this virus is that some of its strains with a high oncogenic risk can lead to the development of cancer, including cervical cancer. An oncologist, obstetrician-gynecologist at the National Medical Research Center of Oncology named after. N.N. Petrova, Ph.D. Olga Alekseevna Smirnova.
– Olga Alekseevna, what is the main danger of the human papillomavirus?
– HPV is a virus that is dangerous for both sexes, since it causes certain associated processes in both men and women. Today, about 200 types of this virus are known to exist, some of them do not pose a serious threat to health, and some can become a risk factor for the development of cancer. HPV types with a high risk of oncogenicity can cause associated processes in the oropharyngeal zone, i.e. mucous membranes of the oral cavity and pharynx, and the anogenital zone - the anal canal and vagina, cervix, vulva, penis. Unfortunately, the incidence of HPV-associated malignant neoplasms has increased among both the male and female population, while among women it is 2.6-3.5 times higher. The problem is very acute. This is the most common sexually transmitted infection. In Central America, the countries of Africa and Eastern Europe, where we include St. Petersburg geographically, the incidence is 20%. If you look at the frequency of occurrence, the most common are types 16 and 18. Unfortunately, the most aggressive type 16 leads in incidence. From the moment of infection, after about 2-3 years, HPV type 16 leads to pre-invasive pathology (oncological process at the initial stage of development).
– Does cervical cancer directly depend on the presence of HPV in a woman?
– If we talk about the development of the oncological process itself, it does not happen all at once – it is preceded by a series of certain pathogenetic factors. On the basis of our Center, a center for cervical pathology and HPV-associated diseases has been created, and a study is underway, the results of which are being prepared for publication. We studied the presence of human papillomavirus in a healthy population and in women with pre-invasive pathology (an oncological process in the initial stage).
– What are the statistics on the incidence of cervical cancer?
– Cervical cancer is the scourge of our time. Every year, 555,100 new cases of this disease are registered worldwide, and 309,800 women die from it. But while worldwide there is a downward trend in mortality from cervical cancer, in the Russian Federation and South Africa the mortality rate from this pathology continues to increase. Today, cervical cancer is one of the leading tumors of the female population of Russia and accounts for 5.3% (fifth place), among those aged 30-59 years - 10% (second place). In the age group of 30-39 years - this is the period of greatest reproductive activity - cervical cancer is the main cause of mortality - 24.4%, and in the age group of 40-49 years it is 15.9%, second only to breast tumors (22.6 %). That is, young women of reproductive age with maximum working potential are most susceptible to cervical cancer. Mortality rates from cervical cancer already exceed those from breast cancer, which led among women under 45 years of age.
– How is HPV transmitted?
– The most common mechanism of transmission is sexual intercourse; contact and vertical are also possible, that is, from mother to child. Low-oncogenic risk HPVs, which lead to the development of genital warts, have the highest degree of contagiousness - the probability of infection for a potential contact is 75-85%.
– How is human papillomavirus determined?
– The test for human papillomavirus is quite simple: a smear is taken from the vagina, this can be done in parallel with traditional cytological studies, the so-called Co-testing. A cytological examination gives a complete picture of the health of the cervix at the moment, and based on the HPV status, a prognostic group is determined, that is, the likelihood of developing pathology. Most often in Russia, PCR testing is used, which determines the presence of the virus, regardless of its clinical manifestation. There are also signal amplification tests that determine the clinically significant concentration of the virus, that is, a threatening level of infection leading to the development of cervical neoplasia.
– How can I get a referral for HPV testing?
– HPV testing must be initiated by a doctor according to the new order for the “obstetrics and gynecology” profile, which comes into force in 2022. You should be aware that HPV testing is not indicated as a screening method for women under 30 years of age. Also, it cannot be an independent screening method in Russia. In fact, any woman should know her HPV status; this is extremely important, since it helps to formulate a follow-up program and not to miss the development of pathology in the future.
– How often should a woman be tested for HPV?
– According to global recommendations, the frequency of examination is once every 3-5 years, depending on age. But often the issue is resolved individually and depends on the woman’s marital status and sexual activity.
– How is men tested for HPV and how often do they need to do it?
– For men, testing for the human papillomavirus is also quite simple: a smear is taken from the urethra and/or anal canal. There is no specific frequency for HPV testing in men, since in this case it is not a screening method, but only a method for identifying a man at risk, but the rate of development of pathology in the male body does not differ from that in the female body. An interval of 3-5 years is considered justified, but it also depends on sexual activity.
– Is it true that HPV can be removed from the body on its own?
– Yes, on average it takes from 12 to 36 months, so when HPV is detected, a woman is monitored at intervals of 6-12 months, depending on the type of HPV.
– How can you protect yourself from HPV?
– There is currently no medicine with proven effectiveness against human papillomavirus infection. There are immunostimulating drugs, but they do not have full proven effectiveness. The only thing we can do for prevention is vaccination. It is most effective at the age of 9-13 years, i.e. before the start of sexual activity. This is a gender-neutral vaccination - it is carried out for both boys and girls. Because HPV-associated diseases can develop in both sexes, and men can also be carriers of HPV. Our goal is elimination, i.e. destruction of the human papillomavirus in the population, then we will be able to eliminate cervical cancer. Secondary and tertiary prevention are screening and treatment. Vaccination of girls is included in the national vaccination schedule in 86 countries; 23 countries have supplemented their programs with vaccination of boys. It is believed that vaccination is too expensive. In fact, if we look at these countries, then, for example, Malaysia, Bhutan, Brunei are not the richest countries, but vaccination coverage there reaches 96-98%. For example, in France, vaccination coverage is only 20%.
– There is an opinion that this vaccine leads to infertility and infects with a virus. How thorough is this?
- This is wrong. The HPV vaccine is a recombinant vaccine, it does not contain live viruses and cannot give you the human papillomavirus. It is registered in 129 countries, approved by well-known world organizations - WHO, International Federation of Obstetricians and Gynecologists, FDA (US Food and Drug Administration). It is considered the safest and most effective vaccine. Regarding infertility, the vaccine protects women from cervical cancer, thus, on the contrary, preserving reproductive function in women.
– At what age can you get vaccinated against HPV?
– Currently, according to updated instructions, vaccination is indicated for men and women aged 9 to 45 years. Vaccination against human papillomavirus infection itself consists of 2-3 stages, depending on age. Today, only the Gardasil-4 vaccine is available on the Russian market; it protects against types 16, 18, 6, 11. There is already a Gardasil-9 vaccine in the world, but it has not yet been approved for use in the Russian Federation. Before vaccination, both women and men need to undergo a test for the human papillomavirus, and women also need a cytological test.
– If a person has HPV, is this a contraindication for vaccination?
– According to the instructions for the drug Gardasil-4, the presence of HPV is not a contraindication for vaccination, but with type 16 HPV, vaccination may no longer have any fundamental clinical significance, but this issue is resolved individually.
– Is vaccination indicated for those who have already been diagnosed with cervical cancer?
- No. Vaccination is prevention, not cure.
– What is the result of vaccination against HPV?
– Vaccination reduces the risk of developing HPV-associated diseases by almost 90%; there is no population-based screening for these diseases. But in Russia, vaccination is not included in the national vaccination calendar, therefore it is carried out only at the expense of citizens’ own funds. What is important: the connection between a carrier of the human papilloma virus and the development of cancer is not subject to state registration; only anogenital condylomas or malignant processes are taken into account. Screening for cervical cancer is extremely important, but it will in no way reduce the spread of the human papillomavirus. The growing mortality rate of women under 45 years of age indicates a steady increase in the spread of cervical cancer and human papillomavirus infection. The solution to this problem lies in the implementation of prevention and screening programs. Therefore, our research and educational work should be aimed at increasing awareness about the presence of HPV, the possibility of vaccination, and the prevention of this pathology in both men and women.
Treatment of cervical papillomatosis
Modern schemes for getting rid of this disease are based on three main points:
- direct removal of formations;
- carrying out antiviral therapy;
- subsequent correction of immunity.
The optimal method for removing papillomas is determined taking into account the size, type, and presence of complications after consultation with a gynecologist. To date, many techniques have been successfully used:
- laser;
- radio wave;
- electrocoagulation;
- cryotherapy with liquid nitrogen;
- exposure to chemical solutions;
- surgical excision.
The question of whether a definitive cure for the papilloma virus is possible remains open. Most doctors agree that, outside of an exacerbation, HPV is not detected by modern diagnostic tools. An alternative point of view is that complex treatment allows you to forget about this disease forever, provided that re-infection is excluded.
Why do you need a cytology test for cervical papillomas?
Cytological examination by Papanicolaou test (PAP test) is the main method for identifying pathological changes in cells and diagnosing precancerous and cancerous pathologies of the uterine cervix.
Material for research is collected from the border of the transition of squamous epithelium to columnar epithelium.
Special brushes and spatulas are used to scrape off the cells, and the resulting cells are placed on a glass slide.
In the laboratory, the sample is stained with two preparations and changes in the cell nuclei and cytoplasm are assessed under a microscope.
The method allows you to determine the nature of the existing changes (inflammation, malignant transformation, reactive changes, etc.).
A specific marker of lesions caused by papillomavirus are koilocytes - cells with uneven large nuclei and vacuoles (normally there are no vacuoles).
Another sign of HPV is the appearance of dyskeratocytes - cells with altered cytoplasm and small dark nuclei.
If cellular changes are confirmed based on the results of the PAP test, a targeted biopsy is performed.
The resulting small pieces of tissue are sent for histological examination.
When cervical papillomas are detected, PCR typing of the virus is recommended in some cases.
This is a determination of the group membership of the pathogen in order to predict the risk of oncological changes.
PCR allows you to detect the virus even in extremely low concentrations.
That is why it is this method that is used to carry out control tests after recovery (including spontaneous).
A relatively new method for diagnosing HPV infection is the detection by ELISA of the E7 oncoprotein in material obtained from the cervical canal.
This protein is normally absent in tissues, and its appearance is due to the activity of HPV.
It is assumed that thanks to such a study it is possible to differentiate between simple carriage of the virus and the initial stages of the processes of tumor change in the affected cells.
Where to remove and treat papilloma in Moscow?
To remove papillomas on the genitals in Moscow, we suggest you use the services of our specialized center for the removal of papillomas at the K-MED laser medicine clinic for the following reasons:
- Latest equipment : At our laser surgery center at the K-MED clinic, we use only the latest surgical or cosmetic lasers. Operations are carried out in a modern operating room, which fully meets all approved standards.
- Experienced doctors : Our center has already existed for more than 15 years. During this time, we have already performed thousands of successful operations. Our dermatologist-surgeons have extensive practical experience in removing skin tumors.
- Removal of papillomas without pain : operations to remove papillomas are performed under local anesthesia, which is selected individually for each specific case.
- Comprehensive treatment : we will analyze the removed tissue to determine the type of virus. After this, our doctors will prescribe you a course of treatment to reduce the concentration of HPV in the body, which will eliminate the likelihood of relapses.
- Transparency of work : before removal, the attending physician will fully tell you how the operation will proceed and discuss the price with you.
- Saving time : we value your time very much, so we will coordinate your appointment time with you in advance so that you do not have to wait. On average, surgery to remove papilloma takes from 20 to 30 minutes.
Get a free detailed consultation by calling (495) 434-34-44 or from 8 a.m. to 8 p.m. daily.
Our addresses : Moscow, Metro Yugo-Zapadnaya or Belyaevo / Konkovo, st. 26 Baku Commissars, no. 6; Moscow, metro station "Proletarskaya" st. Talalikhina, 2/1, bldg. 5.
How to detect malignant changes?
It is not difficult to detect changes in the cervix, but they are not visible to the naked eye. During a routine examination, the cervix may look completely unchanged, therefore colposcopy (examination of the cervix through a microscope) with a vinegar test and a test with Lugol's solution is a necessary part of the initial examination of women, as well as a cytological smear from the cervix. These studies must be repeated once a year (some authors consider it necessary to visit a gynecologist every six months), especially after self-healed erosions, after treatment with medicinal tampons and treatment with liquid nitrogen, regardless of the presence or absence of complaints. It is in these cases that cell degeneration can occur, especially when a viral infection is attached. So the presence of HPV itself is a sufficient risk factor.
Another necessary diagnostic method, as with any viral infection, is the PCR method. This method detects different types of HPV. It has been shown that different types have different oncogenicity, that is, they lead to the development of cervical cancer with different probability. Based on this, high-oncogenic and low-oncogenic were identified. However, it is in the diagnosis of human papillomavirus, unlike the diagnosis of other infections, that PCR diagnostics should not be decisive. As you know, analyzes are also sometimes erroneous. The basis for treatment is primarily the patient’s complaints. And if the clinical manifestations of sexually transmitted diseases are often nonspecific, and PCR diagnostics are carried out precisely to help the doctor identify the exact pathogen and select therapy not at random, but taking into account the sensitivity of this pathogen to specific drugs, then the clinical manifestations of the papilloma virus are obvious and specific, and in case of doubt, the final diagnosis can be made by histological examination. The PCR method is simply not needed in this case. And here's why: if you have condylomas, it's the human papillomavirus. If they are not there, then even if HPV is present in the body (and is detected by PCR), it still does not require treatment. Viruses live in the body for years, integrate into cells, change their genotype and cannot be treated
. Their external manifestations may change and be treatable, but not the presence of the virus in the body. Therefore, if at the time of examination there are no clinical signs of the papilloma virus, PCR diagnostics is not needed, because there is nothing to treat. In cases where there is suspicion of the presence of HPV in the body (if the PCR is positive or the papillomas were previously present or the partner has), observation, repeat colposcopy and cytology are indicated, and, if indicated, histology.
What do these diseases have in common?
Both endometriosis and cervical papilloma are accompanied by changes in the structure of its tissues, and upon examination, the doctor discovers areas of unusual color on the cervix and an uneven surface of the mucous membrane. He can establish a specific diagnosis only after colposcopy and additional examinations, and at the stage of diagnostic search he only assumes the presence of papilloma or proliferation of endometrioid tissue.
What unites these two pathologies is the fact that they often cause intermenstrual spotting, bloody vaginal discharge, including those that appear after sexual intercourse, and a feeling of pain during it. That is, there is a certain similarity in symptoms.
How to treat and how to live with it?
In the absence of manifestations of HPV, the carrier is still contagious and transmits the virus to others. So there is no point in worrying about this - most young people are infected with HPV. It's not scary. Let us repeat: the virus is dangerous only when it manifests itself on the cervix or glans penis. There it has oncogenic activity and requires treatment. In other cases, this is more a cosmetic problem than a medical one. If there are clinical manifestations of the virus, PCR is especially not necessary; the general algorithm for managing patients with papilloma virus is included: colposcopy, biopsy, treatment. The criterion for choosing treatment is the severity of dysplasia (i.e., changes in cells on the cervix), and not the type of virus. Severe dysplasia and a low-oncogenic type of virus require treatment. The highly oncogenic type and the absence of dysplasia do not require surgical treatment.
HPV poses an oncogenic danger only to the cervix and glans penis. Papillomatosis of the skin, vagina, and external genitalia is not dangerous from an oncological point of view, and its treatment depends on the severity of the cosmetic defect, the patient’s desire and the severity of itching, a frequent companion of the papilloma virus. It should be remembered that surgical removal is not a treatment for papillomatosis, but only the removal of altered tissue. The virus will remain in the blood, with a decrease in immunity, genital warts will form again, and the person will continue to infect others. This does not mean that there is no need to remove condylomas; it means that when they reappear, you should not think that you were poorly treated or were re-infected. This is your virus, and you have to live your life with it. There is nothing scary about this, you just need to lead a healthy lifestyle, maintain your immune system and monitor places that are dangerous from an oncological point of view (the cervix or the head of the penis).
Other articles by the author
- Endometrial polyp
- Bacterial vaginosis
- Adenomyosis of the uterus
- Painful periods
- Human papillomavirus and cervical cancer
- Vulvitis
- Vulvovaginitis
- Hormonal disorders
- Cytomegalovirus
- Endometritis
- Endometriosis
- Cervical erosion
- Chlamydia
- Trichomoniasis in women
- Hidden infections
- Female infertility
- Adnexitis, inflammation of the appendages
- Urinary incontinence in women
- Bartholin gland cyst