Human papillomavirus, commonly abbreviated as HPV.
This is the causative agent of the most common infectious pathology of mucous membranes and skin throughout the world, the so-called. papillomavirus infection.
There are about 200 types of this virus.
About a fifth of which can be transmitted through sexual contact, damaging the organs of the urogenital system.
This pathogen is of particular concern due to the connection between infection and cancer pathologies.
Thus, 93% of episodes of cervical cancer in women are caused by this particular virus, of which 70% are HPV types 16 and 18.
That’s why, if a woman’s HPV 16 is detected in tests during an examination, the doctor strongly recommends additional studies.
So what is it: HPV 16 genotype in women?
All papillomaviruses are conventionally divided into three main groups depending on their oncogenic danger:
- non-oncogenic, causing flat/plantar/vulgar warts (types 1, 3, 2, 4, 41, 10, etc.), not capable of causing malignant transformations
- low risk, causing the development of anogenital warts (otherwise called genital warts), resembling characteristic cauliflower buds, epidermoplasia verrucous, laryngeal papillomatosis (types 5, 17, 12, 6, etc.), can extremely rarely, under very “favorable” conditions, cause malignant process
- high risk, capable of causing neoplastic changes in women in the area of the uterine cervix, bowenoid papulosis (HPV types 16 and 18, 33, 31, 39, 35, 58, 56, 45, 68, 59, 52, 51), have been proven to provoke the overlap of various factors oncological processes
Thus, the answer to the question of whether HPV 16 infection is dangerous for a woman’s health has been determined: it is this type of virus that poses a serious threat.
However, the presence of a pathogen does not mean the presence of a disease.
In addition, HPV infection has an interesting feature: the ability to self-heal.
That is why in a situation where a certain amount of HPV type 16 DNA is detected in women during laboratory tests, it is important not to panic.
You just need to follow your doctor's recommendations and undergo regular examinations with a gynecologist.
results
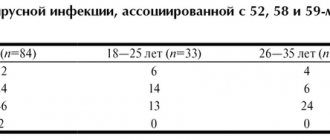
79.8±4.4% of patients in the observation group were under the age of 35 years (inclusive). The distribution of cervical infection with HPV types 52, 58 and 59 depending on age was as follows: early reproductive age (18-25 years) - 33 patients, middle age (26-35 years) - 34, over 36 years - 17.
An analysis was carried out of the frequency of HPV-associated lesions of the cervix, which are divided into clinical (exophytic condyloma), latent (lack of clinical, morphological changes when HPV DNA is detected), subclinical form (invisible to the naked eye, asymptomatic, detected only by colposcopy and/or morphologically) , CIN I-III degrees and cervical cancer [1]. There were no cases of clinical PVI. Among the infected women, there were patients with CIN (46-54.8%), a relatively latent form of infection without clinical manifestations (12-14.3%), a subclinical form of infection (24-28.6%) and cervical cancer (2-2 ,4%).
Depending on the severity of the histologically verified precancer, CIN I was detected in 51.2%, CIN II in 32.5%, and CIN III in 16.3% of cases.
When analyzing the frequency of forms of PVI associated with the types studied depending on age, attention was drawn to the absence of significant differences in the latent form in all age groups ( p
>0.05) (Table 1).
In turn, in the presence of cervical pathology, the influence of the age factor is clearly manifested. Thus, the subclinical form of PVI was dominant in patients of early reproductive age compared to that in patients aged 26–35 years ( p
= 0.05), in whom a predominance of CIN was noted (
p
= 0.02).
There were no significant differences in the severity of CIN (grades I–III) depending on age. Two cases of cervical cancer associated with HPV type 58 were observed in a group of women over 36 years of age. A direct, weak, statistically significant correlation between the form of PVI and age was established (rS=+0.21; p
=0.0517).
Table 1. Forms of human papillomavirus infection associated with types 52, 58 and 59, depending on age
When studying the nature of infection (mono-, combined), it was found that infection of the cervix with the participation of one of the studied types of HPV was observed in 37 (44 %) of patients: type 52 - in 19, type 58 - in 13, type 59 - in 5 (Table 2). In 44 (52.4%) women there was a combination with other types of HR HPV 16, 18, 31, 33, 35, 39, 45, 51 and 56 (the most common types were 16, 31 and 56), in In three cases, a combination of two of the 52, 58 and 59 types was noted.
Table 2. Frequency of detection of HPV types 52, 58 and 59 in women with PVI
Particular attention was paid to monoinfection of the studied HPV types. Among 37 women in whom one of the types was identified (52, 58, 59), the distribution of forms of the disease was as follows: latent - in 5 patients, subclinical - in 12, CIN - in 19, cancer - in 1. Cervical neoplasia (CIN and cervical cancer) amounted to 20 (54%) cases with monoinfection, and 28 (59.6%) cases with the combined form, which did not have statistically significant differences ( p
=0.3973). Frequency of CIN with monoinfection of type 52 - 6 observations out of 19 of this type, with monoinfection with HPV type 58 - 10 out of 13, with monoinfection with HPV type 59 - 3 out of 5 observations, CC (1 case) - with monoinfection with HPV 58 type (Fig. 1).
Rice.
1. Distribution of HPV-associated lesions of the cervix in mono- and combined forms of infection. The viral load of HPV types 52, 58 and 59 was assessed among 84 infected women (including mono- and co-infection) (Table 3). In 30 cases, its level was below the threshold of clinical significance, in 30 cases the viral load of HPV types 52, 58 and 59 was in the range from 3 to 5 lg per 105 cells, in 33 cases the viral load was above the progression threshold. Exceeding the progression threshold varied in the range of 25–46.7% depending on the HPV type (Fig. 2).
Table 3. Distribution of viral load levels by HPV type in the group of examined patients (mono- and combined infection) Note. *Here and in the table. 4: the number of viral load observations did not coincide with the number of patients examined due to co-infection.
Rice. 2. Viral load of HPV types 52, 58 and 59 in women with PVI.
When analyzing the relationship between clinical forms of PVI and the level of viral load, a twofold excess of cases with a load exceeding 5 lg per 105 cells was found in women with CIN: 25 versus 10 (less than 3 lg per 105 cells) and 11 (from 3 to 5 lg per 105 cells) cases, p
=0.0091 (Table 4).
Table 4. Dependence of the form of PVI in HPV types 52, 58 and 59 (mono- and combined infection) on the viral load.
In the case of monoinfection, the latent form was not accompanied by a load above the progression threshold, the subclinical form occurred against the background of exceeding the progression threshold in 1 case against the remaining 11, while CIN and CC - in 13 versus 7 cases with a lower viral load (Table 5). A statistically significant relationship was established between the severity of PVI and the level of viral load of types 52, 58 and 59 (2I=16.29; p
<0,05).
Table 5. Forms of PVI in monoinfection with HPV types 52, 58 and 59
According to studies based on large clinical material, among various age groups, an increase in the level of viral load increases the severity of HPV cervical damage [5, 20, 22-24]. According to a study by G. Shen et al. [25], a positive correlation was noted between the level of viral load and the degree of cervical lesions. Our data proves the influence of the viral load for HPV types 52, 58 and 59 on the progression of cervical neoplasia.
Where does HPV type 16 come from in women?
According to WHO, up to 80% of the population is infected with HPV.
But only about 10% of those infected have clinical manifestations.
The answer to the question of how HPV 16 is transmitted to women is well known: the main route of infection is sexual contact.
Including anal-genital and oral-genital, with an infected partner.
HPV has a very high prevalence: almost 80% of women by the age of 50 have been infected at least once.
At the same time, the virus has a tendency to self-eliminate.
So it is not possible to establish the probability of infection after a single contact.
This is why it is so important not to neglect preventive measures during casual sexual acts.
Infection of a child by the mother at the time of birth is possible with viruses of types 6 and 11 - the cause of such a disease in children as respiratory papillomatosis.
No other types of virus, including HPV type 16, usually cause problems during pregnancy in either women or newborns.
There are only isolated cases of infection of newborns by mothers with bowenoid papulosis.
Therefore, routine HPV testing is not recommended by any international/national guidelines.
The incubation period varies from three months to several years.
It is possible to become infected with several types of viruses at the same time.
After entering the body, the virus infects the tissue covering the surface of the body and organs - the epithelium, namely its inner part (basal layer).
The virus inside the cell may not affect chromosomes or integrate into the genome.
The last option, the so-called. the malignant form is manifested by the appearance of cells with altered DNA, which multiply and form a tumor.
Thus, if a woman is a carrier of HPV type 16, 18, 6, 11 or others, the following conditions are possible:
- latent course of infection, when the virus does not affect cellular DNA, women have no clinical manifestations, and infection is detected only by PCR
- the appearance of such clinical manifestations as condylomas, warts, papillomas, the virus does not change the cellular genome, but provokes increased cell proliferation (the problem is detected by the presence of symptoms, PAP test, PCR method)
- the development of neoplastic changes (dysplasia), when the virus made a change in the DNA of the cell and caused corresponding changes in the latter (such changes are called koilocytosis), the situation is confirmed by PCR, PAP test, histological and colposcopic examination
- carcinoma, when the pathogen has changed the cellular genome and caused the formation of a large number of altered (“atypical”) cells – invasive cancer (the diagnosis is confirmed by PCR, Pap test, histological and colposcopic studies)
In most situations (up to 90%), the body heals from the virus within about 2 years.
The development of symptoms is observed only in 1-5% of infected people.
With regard to HPV 16, causes of severe clinical symptoms in women include:
- early onset of sexual activity
- having multiple sex partners
- multiple pregnancies/births before age 20
- smoking
- chronic cervicitis
- decreased immune defense, for example, due to concomitant HIV infection (with a normal functioning immune system, cancer in an infected woman can develop in 15-20 years, while in an HIV-infected woman - in 5-10 years, while HIV also increases the likelihood HPV infection)
Prevalence
- 1Hapillomavirus infection is the most common sexually transmitted infection.
- 2Among the sexually active population, more than 50% are infected.
- 3The likelihood of infection with the human papillomavirus increases with the number of sexual partners.
- 4Non-genital skin warts are most common among adolescents, as well as adults working with meat products (incidence rate - 10%).
- 5 Papillomavirus most often affects women: the virus is detected in 22-35% of women and 2-35% of men. The incidence ratio among women and men is 1.4:1.
- 6Oncogenic strains cause about 5% of all cancers in the world.
Manifestations of HPV infection
In most situations, when infected with HPV in general and, in particular, HPV 16, women, as well as men, have no symptoms.
Sometimes a sign of infection can be warts and condylomas (in the case of the presence of a virus from the low-oncogenic/non-oncogenic group).
With HPV 16 infection, women may experience precancerous changes on the cervix.
This is revealed during a gynecological examination.
Or preventative, or when the patient consulted a doctor for another reason, for example, with complaints of unusual discharge.
The main diseases caused by HPV 16 are bowenoid papulosis and dysplasia of varying degrees.
With bowenoid papulosis, dense brownish, reddish or flesh-colored papules appear in the labia, pubis, inguinal and perianal areas.
They merge into large warty surfaces up to 2 cm in diameter.
The disease is characterized by a chronic, long-term course.
Malignancy develops in 3% of episodes (degenerates into squamous cell carcinoma), although self-healing is more often diagnosed.
Cervical dysplasia is a precancerous change and requires serious consideration.
Since this pathology may not be diagnosed in a timely manner due to its asymptomatic course, most countries in the world have adopted cervical cancer screening programs.
There are several classification approaches for dysplasia and cervical cancer.
They are based on the results of morphological/cytological studies (studies of cell changes).
According to the International Classification of Diseases, 10th revision, there are:
- mild dysplasia - minor proliferation and changes in epithelial cells, often a similar condition is detected during inflammatory processes in the uterine cervix and is eliminated after appropriate anti-inflammatory therapy
- moderate dysplasia - changes affect the entire lower layer of the epithelium
- severe dysplasia - the entire length of the epithelium is affected, the cell structure is noticeably changed
- cervical cancer (otherwise known as squamous cell carcinoma) – detected during colposcopic examination, confirmed cytologically and histologically
Moderate and severe dysplasia in most episodes is caused by exposure to the virus.
Signs of cervical cancer are detected only in the last stages and include:
- bleeding between menstrual periods, irregular, after sexual intercourse
- unpleasant smell of discharge
- vaginal discomfort
- pain in the pelvic area, back, legs
- weight loss
- fatigue, lack of appetite
- unilateral swelling of the legs
As the disease progresses, the severity of symptoms may increase noticeably.
conclusions
1. Among the cohort of women with human papillomavirus infection of the cervix associated with HPV types 52, 58 and 59, a significant proportion of women are under 35 years of age (79.8%).
2. The age-dependent nature of the frequency of subclinical infection and cervical neoplasia in infected women has been established.
3. Human papillomavirus infection associated with HPV types 52, 58 and 59 was accompanied by the presence of CIN and cervical cancer in 57.1% of cases.
4. High frequency of cervical neoplasia during monoinfection (54%), comparable to its frequency when combined with other types of HR HPV (59.6%; p
>0.05), as well as the relationship between the severity of the lesion and the level of viral load, confirm the high risk of the formation of precancer and cervical cancer in the presence of monoinfection with HPV types 52, 58 and 59.
Diagnosis of HPV infection
Anogenital warts, caused by viruses type 6 and 11, are easily detected during a gynecological examination.
Identification of such formations is an indication for additional examination of the uterine cervix, and, if necessary, the urethra (urethroscopy).
The main method for detecting neoplastic changes caused by HPV is the Pap test.
It is a cytological study of smears from the uterine cervix.
In general, oncocytology is a method for detecting cancer cells in the cervix and vagina.
Samples of material for study are taken during a gynecological examination using special cyto-brushes and are absolutely painless.
A distinction is made between simple oncocytology, when the cells under study are immediately applied to slides for microscopy.
And liquid, when the cells are pre-treated with a special solution and dye.
The latter type is the PAP test.
After processing the material with two types of dyes, changes in the cell nuclei and cytoplasm are easily detected in the sample using microscopy.
The type of pathological process is preliminarily determined: inflammatory, malignant, or other.
Then, based on the severity and nature of the changes, a differential diagnosis of possible conditions is carried out.
The PAP test is included in the screening system for detecting cervical cancer in all developed countries.
Its annual holding is recommended for all females who have reached the age of 20 years.
Cytological signs of HPV infection include:
- koilocytosis - the appearance of characteristic koilocyte cells with voluminous uneven nuclei, vacuoles (absent normally) and clearing zones near the nuclei
- dyskeratocytosis - the appearance of keracite cells with dark nucleoli and characteristically altered cytoplasm
If the PAP test reveals a change in cellular structures, the following is carried out:
- colposcopic examination with acetic acid examination and test with Lugol's solution
- histological examination – small fragments of tissue are studied under a microscope (the latter are obtained by targeted biopsy)
Colposcopic signs of infection:
- lightening of areas treated with acetic acid
- uneven staining with Lugol's solution
- the presence of characteristic outgrowths (for low-oncogenic types of the virus)
According to international recommendations, diagnostic tactics for detecting disorders using the PAP test include:
- The first option is to repeat the examination after three months, in case of normality, repeat after six months and a year, in case of abnormality - colposcopic examination
- The second option is to immediately conduct a colposcopic examination; if no abnormal abnormalities are detected, cytology is repeated six months later (for oncogenic types of the virus). If necessary, a biopsy and canal curettage are performed. In a situation with insufficient reliability of colposcopic data, anti-inflammatory, estrogen therapy is recommended, followed by repeating the study
- The third option is to determine the type of virus using the hybrid capture method (the so-called Daijin test, Digene) or PCR (polymerase chain reaction). Detection of HPV type 16 or another oncogenic virus in women (the norm is the complete absence of the pathogen) is an indication for colposcopy
Typing of papillomaviruses by PCR has a high diagnostic value in terms of determining the type of virus and its belonging to a high-risk group of oncology.
Also to predict the likelihood of developing cancer against the background of existing neoplastic changes in the cervical epithelium.
Qualitative analysis produces a result in the format “there is a virus of this type / not.”
The quantitative method (real-time PCR) allows you to detect viral DNA even in very low concentrations from 10 to 100 copies in a sample.
Can be used to track the dynamics of infection.
Due to the fact that young women have a high rate of self-healing from HPV, PCR is recommended to determine the type of virus only after the age of 30.
A blood test to determine antibodies to HPV has no diagnostic value and is carried out only for research purposes.
As for the problem of preferring the Digene test or PCR, it is important to consider that the first method determines the number of HPV type 16 and other types in women from 5000 copies.
Whereas PCR “senses” a significantly lower content.
This point is significant from the point of view that this is the number that is clinically significant.
Those. More than 5,000 copies were detected against the background of neoplastic conditions - a high risk of oncology.
And detection of a smaller amount does not allow predicting the risk of developing cancer against the background of dysplasia.
In general, the analysis data allows the doctor to decide whether to start treatment or limit himself to observation.
Screening and treatment of precancerous lesions of the cervix
Screening
Cervical cancer screening involves testing for HPV infection to identify precancerous lesions, followed by appropriate treatment. Testing is carried out among women who have no symptoms and feel completely healthy. If screening detects HPV infection or precancerous lesions, they can be easily treated and thus prevent the development of cancer. Screening can also detect cancer at an early stage, when there is a high chance of cure.
WHO's updated guidance now recommends that countries use HPV tests for cervical screening, including:
- HPV DNA tests, which detect highly dangerous strains of HPV that cause almost all types of cervical cancer;
- HPV mRNA tests to detect HPV infections that lead to the appearance of atypical cells.
HPV tests, unlike visual examinations, provide an objective result. They have proven to be easy to use, detect more precancerous and cancerous conditions, and save more lives. Their use is also more economically justified compared to visual examination methods or cytology (Pap smear).
In the general population of women, screening should be performed using a validated HPV test starting at age 30 at intervals of 5 to 10 years; Among women with HIV infection, it should be carried out starting at 25 years of age. In addition, HIV-infected women should be screened more frequently, every 3–5 years.
To perform cytology and HPV testing, medical personnel use similar procedures for collecting a cervical sample. WHO allows patient self-sampling when testing for HPV DNA (but not mRNA). Women must be given adequate support to complete this procedure with confidence.
Screening should be linked to the treatment and management of patients with positive screening results. HIV-positive women in resource-poor settings may be prescribed treatment without confirmatory diagnosis. However, treatment for HIV-positive women can begin only after receiving a positive test result for HPV (for example, visual examination using acetic acid).
Treatment of precancerous conditions
If it is necessary to treat precancerous lesions and the patient meets the treatment criteria, it is recommended to remove the affected tissue using cryotherapy or thermal ablation. Both treatments are effective and safe and can be performed on an outpatient basis.
If the criteria for ablative treatment are not met or if cervical cancer is suspected, the patient should be referred to a specialized medical facility that has the capabilities to conduct proper examination using colposcopy and biopsy. If necessary, she may undergo excision (LLETZ), and in the case of cancer, an individualized treatment plan can be developed taking into account the stage of the disease, the patient's health status and preferences, as well as the availability of medical resources.
Treatment of HPV infection
Which doctor treats HPV 16 in women?
Treatment of HPV infection can be carried out by a gynecologist, oncologist, infectious disease specialist, or venereologist.
It is important to understand that accidental detection of the virus in the absence of clinical changes is not an indication for therapy.
Only if highly oncogenic viruses (HPV 16) are detected in women, the doctor decides what to do next.
Is it necessary to undergo diagnostic examinations and examinations more frequently or to prescribe additional studies?
Only a specialist can determine whether it is necessary to treat HPV 16 in women, taking into account the presence/absence of changes induced by the virus.
In a situation with HPV, it is important to trust your health only to highly professional specialists who are familiar with international protocols for managing the infection.
This is especially important when infected with HPV 16, which provokes malignant pathologies in women (reviews on the Internet or from friends will help you decide on an institution and a doctor).
Today, in women, treatment for HPV 16 is based on the removal of atypically changed epithelium.
It should be understood that if women have an infection, there are currently no drugs that destroy the virus itself.
Any international treatment regimen for HPV 16 does not include any antiviral agents.
At the same time, specific treatment for HPV 16 is carried out, in which it is recommended that women take drugs with immunomodulatory and antiviral activity.
It is believed that such drugs mobilize the immune system to fight the virus.
Such products have not been sufficiently tested for effectiveness in clinical trials.
Accordingly, there is no reliable data on the cure rate.
Despite this, many patients note a significant improvement in their well-being after using them.
Immunocorrective therapy for HPV 16 in women includes:
- with human recombinant interferon or its inducers, suppositories (Viferon, Genferon), Isoprinosine, Cycloferon, etc.
- with an immunostimulating effect - Lykopid, Polyoxidonium, etc.
- B vitamins, omega acids and dietary supplements
Often, before prescribing a drug treatment regimen, an analysis of the immune status (immunogram) is recommended.
With determination of indicators of the activity of monocytes, neutrophils, lymphocyte function, levels of immunoglobulins, CD16+, CD8+, CD4+ and others.
Unfortunately, for many drugs, data on the safety of use, complications and relapses after use have not been obtained.
Therefore, it is recommended to refrain from using them for people with:
- autoimmune diseases
- malignant formations (for cervical cancer can be prescribed only after completion of surgical treatment)
- allergic reactions
- bronchial asthma, etc.
As for the generally accepted approach to the management of HPV infection in the international medical community, the following points are positioned here:
- There is no medicine to remove the virus from the body, but the likelihood of self-healing is very high, especially at a young age
- If there are no changes in cellular structures and a virus from a high oncogenic risk group is identified, more frequent and careful monitoring of the patient is carried out
- If changes caused by the activity of the virus are detected, therapy is carried out aimed at eliminating pathological changes
For bowenoid papulosis caused by HPV type 16, tumors are removed using the following methods:
- Mohs excision
- laser therapy
- cryodestruction
- electrocoagulation
- local application of ointments with cytostatics (5-fluorourocil, prospidin, fluorofur)
- intralesional administration of interferon
- oral administration of Neotigazon capsules
Precancerous conditions and the first stages of cervical cancer are highly treatable.
The changed cells are removed using cryotherapy.
For dysplasia, organ-preserving operations are performed: conization of the cervix with a scalpel, electrosurgically, laser with preliminary canal curettage.
For localized forms of the tumor, surgical treatment is carried out, for a widespread process - radiation and chemotherapy.
Taking into account the fact that eliminating the result of virus activity does not remove the infectious agent itself.
The risk of recurrence of pathological changes remains, which, in turn, requires further monitoring of the patient.
In addition, the possibility of HPV reinfection cannot be excluded.
After implementing any treatment option, follow-up tests are recommended.
Since there is a possibility of spontaneous elimination of the virus within 2 years from the moment of infection.
A separate problem is presented by persons with HPV against the background of HIV infection.
It has been proven that the risk of developing cancer in such women is higher, as is the risk of HPV infection itself.
Although primary HPV infection was detected more often, which is associated with the greater prevalence of this virus.
Moreover, the worse the patient’s immune status, the higher the likelihood of her developing HPV-induced cancer.
Therefore, people with HIV status are recommended to undergo HPV testing more frequently.
Treatment is carried out using the same methods as for those uninfected with HIV, with additional specific therapy aimed at suppressing the activity of the immunodeficiency virus.
What are the consequences of HPV during pregnancy?
To date, there is no reliable evidence of a pronounced negative impact of infection on the course of pregnancy.
Pregnancy pathologies such as miscarriage, premature birth, etc., which are characteristic of other sexually transmitted infections, have not found unconditional confirmation of the connection with HPV.
However, if a woman’s primary infection occurs during pregnancy, there is a risk of developing various complications.
Anogenital warts in the mother caused by HPV types 6 and 11, localized in the area of the labia minora and the vestibule of the vagina, have some consequences for the fetus during pregnancy.
Such genital warts carry a small risk of infection of the fetus during childbirth, leading to the development of respiratory papillomatosis in the latter.
Respiratory, or otherwise laryngeal, papillomatosis (also called laryngeal papillomatosis) most often develops in children 2 to 3 years old.
As a result of infection from a sick mother during the latter’s pregnancy or immediately at birth.
The route of transmission during pregnancy through the placenta, during childbirth or immediately after it is not yet entirely clear.
The main symptoms of the disease are hoarseness, up to the complete disappearance of the voice, and difficulty swallowing.
As the disease progresses, shortness of breath and cough appear.
In severe situations, blockage of the upper respiratory tract and asphyxia are possible, especially in the case of formations with a long thin stalk.
During examination using a laryngoscope (sometimes a bronchoscope is also used), typical growths - condylomas - are found on the laryngeal mucosa.
This pathology has a rather aggressive course: after removal of the formations, relapses often occur, requiring repeated surgical interventions.
If pregnancy occurs due to infection with highly oncogenic papillomaviruses (especially HPV 16, 18), the woman must inform her obstetrician-gynecologist about the presence of infection.
The fact is that changes in a pregnant woman’s body can provoke more intense cell transformation.
Actually, such viruses do not affect the course of pregnancy itself or the child, but they pose a certain threat to the woman’s health.
In a situation where no infection was detected in the past, a cytological Papanicolaou smear (Pap test) is taken, among others, when registering.
If the analysis shows abnormalities, the doctor prescribes additional tests (for example, colposcopy).
Also, situations when pregnancy occurs in women with erosion require special attention.
PCR diagnostics are required to exclude infection with high-oncogenic risk HPV.
As a rule, in the routine practice of an obstetrician-gynecologist, such a combination as HPV and pregnancy is not specifically examined.
Tests for the virus are recommended only if pathological abnormalities are detected.
At the same time, there are research studies demonstrating the effect of the virus on pregnancy.
Thus, it has been shown that infection of women with HPV slightly reduces the likelihood of embryo implantation, and in men it reduces sperm motility.
And since in a married couple, as a rule, both partners are infected, the onset of pregnancy is associated with some difficulties.
As a result, when planning a pregnancy against the background of an infection caused by HPV, planning an IVF procedure, this factor should also be taken into account.
Diagnostic measures
Early detection of HPV type 16 infection is only possible using molecular diagnostics.
It allows you to establish unique DNA sequences that are unique to the desired papillomaviruses.
For this, three types of techniques are used:
- non-amplification
- amplification (PCR)
- signal amplification (hybrid trap system - Digene Hybrid Capture System II)
Tests of the first type are not used in practical medicine due to the high cost and complexity of their implementation.
Amplification methods, among which PCR is the most studied, are used quite widely and are well studied.
Allows you to establish the fact of infection with HPV 16.
They detect viruses of other types (it is quite possible to become infected with several representatives of papillomaviruses at the same time).
The real-time PCR technique also determines the DNA concentration of oncogenic viruses.
This indicator has important prognostic value in dynamics.
Initially large numbers at the start of treatment should gradually fall under the influence of special therapy.
And completely disappear after any destructive treatment or surgery.
If the concentration of viral DNA in the diagnostic material is initially low, the doctor may recommend a wait-and-see approach.
Sometimes there is a 20% chance that HPV type 16 with a low DNA concentration will spontaneously clear from the lesion.
Digene (or Daijin test) differs from PCR in its unprecedented accuracy and high speed of testing (within one day).
Daijin also allows you to perform a quantitative analysis (calculate the concentration) of viral DNA.
The only thing holding us back from introducing this technique into widespread clinical practice is the significant cost of research.
To conduct such rather complex and high-tech tests, a man should contact doctors with access to modern laboratory centers.
The use of oncocytology, the most well-known method for diagnosing tumor processes, is justified only for developing treatment tactics for a man.
The method allows you to determine whether the tumor cells have degenerated into a malignant process or whether the papilloma still remains benign.
This information, provided by oncocytological examination of a tissue sample from a suspicious lesion, is decisive for the development of treatment tactics.
An immunogram in its classical concept is of little value for diagnosing HPV type 16 infection in men.
With its help, you can only establish the approximate duration of infection - based on the types of immunoglobulins identified.
IgA and IgM are detected with recent infection, and IgG - when infection is several months old.
Therapeutic measures
Considering the high risk of developing a malignant tumor at the site of HPV 16 infection, all men with a confirmed diagnosis need to be treated.
Regardless of the concentration of pathogens.
Especially if the formation is large enough and/or located in the urethra, it interferes with urination.
The exception is when small concentrations of viral DNA are detected with small papillomas.
This gives a certain chance for independent recovery.
Moreover, it is necessary to ensure regular monitoring of the condition of papilloma.
But even here, according to individual indications, the doctor may still recommend treatment.
There are three general approaches:
- removal of external manifestations of infection - viruses are also removed along with the affected cells
- conservative treatment - the use of various types of drugs and preparations, both local and systemic
- combined approach – a balanced combination of surgical and conservative components
As a rule, the best effect is achieved using the third approach.
Therefore, it is better for a man to immediately assume that he will have to be treated in at least two institutions.
Surgical profile for the stage of papilloma removal and therapeutic profile - to consolidate the achieved results.
It will also be necessary to undergo periodic examinations to ensure the effectiveness of treatment or to detect early signs of relapse.
Everything is done on an outpatient basis, without wasting time and money.