Classic alopecia. Androgenetic (male) and diffuse (female) alopecia
These are the two most common situations in medical practice. The cause of androgenetic alopecia (AGA) is most often genetics, followed by provoking factors: stress, lack of microelements, vitamins, trichotoxic drugs, etc. Therefore, more often we call AGA not a disease, but a pathological condition.
What is characteristic of the female type of hair loss is that, in addition to genetics, hormonal problems (usually sex hormones) are in second place, and in this case, alopecia can often occur after various diseases.
Now let's look at the effect of provoking factors in more detail.
Hair and scalp diseases
What are the causes of alopecia? What is the differential diagnosis for focal baldness? How to manage patients with scalp psoriasis?
The problem of hair loss - diffuse or focal - and scalp diseases are the most common reasons for referral to a dermatologist. Hair is an important part of our body, and any damage to the hairline is associated with inconveniences that we are not inclined to underestimate.
| Figure 1. Bilateral receding hairlines characteristic of male pattern baldness. A new drug has recently been licensed - finasteride. |
There is an opinion that hair serves as a symbol of fashion and sexuality. People without hair seem unattractive to us and look unusual. Men feel less “masculine” and experience insecurity in their personal relationships and at work.
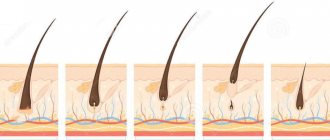
Hair goes through a cycle of growth (anagen) and loss (telogen); Normally, up to 100 hairs fall out per day. Only when this figure is exceeded does hair loss become noticeable. There is also a seasonal dependence: more hair is lost in summer than in other seasons.
- Diffuse baldness
Telogen effluvium hair loss. Diffuse alopecia can develop after a serious illness or surgery and can be quite severe. As a rule, two to three months after childbirth or illness, a large amount of hair shifts from anagen to telogen and falls out. This manifests itself as excess hair loss, but not complete baldness, and it is important to reassure the patient that the hair will grow back. The same thing is observed after exhausting diets.
The nature of hair loss after a course of chemotherapy differs from that described above, since it occurs in the anagen phase. Iron deficiency and thyroid disease can also lead to diffuse hair loss.
Androgenic alopecia. Up to 60% of women over 30 experience some degree of male pattern baldness, and the incidence increases after menopause.
As in men, the frontal part and crown of the head mostly go bald; Once again, women need to be reassured that this type of hair loss is rarely severe. However, receding hairlines do not tend to grow over. Minoxidil lotion helps slow hair loss, but although 30% of patients experience some improvement, only 10% of men and women achieve effective hair restoration.
This expensive treatment is not available under the national health care system. In addition, the effect of this treatment lasts only during the use of the drug, then the hair condition gradually returns to its previous state.
Androgenetic alopecia develops to some extent in women with polycystic ovary syndrome, they also have acne, hirsutism and irregular periods. For hormonal disorders, cyproterone acetate at a dose of 50-100 mg per day in combination with estrogen, as in the Diane contraceptive pills, helps well.
Men with androgenetic alopecia begin to lose hair from the temples and then from the crown. The severity of baldness varies widely. The number of men with this type of baldness increases with age, until by the age of 70 it reaches 70%.
| Figure 2. Up to 60% of women over 30 years of age suffer from male pattern baldness to varying degrees. |
As a rule, there is a family predisposition to this type of baldness, and most men perceive it as an attribute of aging. For those who feel differently about this, we can recommend minoxidil; There are many clinics, often illegal, offering hair transplants and implantation. Baldness is a problem that many people seek to make money from. Finasteride, a 5-a-reductase inhibitor, has recently been licensed for use in androgenetic alopecia in men. It is taken orally, but there may be side effects such as loss of libido or impotence.
Many teenage girls and young women who complain that their hair is falling out and thinning actually have beautiful hair with no signs of thinning. It looks like the thick thick hair they had in
| Figure 3. Alopecia areata can develop at any age and in both sexes, but it is more common in adolescents and young adults. |
childhood, they simply come to a state corresponding to a different age norm. No objective reasons have been found for this phenomenon, but although we do not know why the hair becomes thinner, girls can be reassured by assuring them that this will not continue indefinitely: soon the condition of their hair will stabilize at a new, completely acceptable level.
- Patchy baldness
Alopecia areata. Patchy baldness usually develops as a result of alopecia areata, an autoimmune disease in which antibodies are produced against the hair follicles. The patient experiences bald areas on the scalp. The beard and eyebrow areas may be involved, and in severe cases, all the hair on the head (alopecia totalis) or body (alopecia universalis) will fall out.
| Figure 4. In tinea capitis, the scalp shows flaking, broken hair, and random patches of baldness. |
Alopecia areata can develop at any age and in both sexes, but teenagers and young adults are more often affected; it may be associated with other autoimmune diseases such as thyroid disease and vitiligo. The scalp is healthy, with smooth, rounded bald patches and characteristic single hairs that look like exclamation marks. In 70-80% of cases, the nests heal spontaneously, but there remains a possibility of relapse: more than half of the patients will develop new areas of baldness over the next five years.
The occipital sockets overgrow worse, and the larger the area of baldness, the less chance of a successful outcome. In 5-10% of cases, the disease ends in total or universal alopecia. Only 10% of patients recover from total alopecia; if hair loss begins before puberty, the prognosis is less favorable. In some patients, small indentations are visible on the nails.
| Figure 5. Dermatomycosis of the scalp. Visible typical greenish-blue glow under Wood's lamp |
Differential diagnosis for focal hair loss includes ringworm and trichotillomania. In the first case, there is flaking of the scalp, and in both cases the hair breaks rather than falls out completely.
For alopecia areata, strong steroid drugs such as clobetasol propionate or topical triamcinolone are used to stimulate hair growth. It is difficult to say with certainty that the overgrowth of lesions occurs due to treatment, since in many cases the hair is restored spontaneously. At least the patient feels that he is being helped, and the use of the ointment for six to eight weeks or periodic injections does not cause skin atrophy.
Some patients are happy to hear that the chances of spontaneous recovery are good and no treatment is required. Typically, hair grows naturally within a year, in most cases within the first six months.
| Figure 6. Trichotillomania. Typically, the patient needs treatment for an underlying mental illness |
In severe cases, a regimen of PUVA (oral psoralen followed by long-wave ultraviolet light), high-dose systemic steroids, and irritants such as dithranol, dinitrochlorobenzene, or diphencipron may be tried. But most often the effect turns out to be too insignificant compared to the severity of the side effect.
Dermatomycosis of the scalp. It develops as a result of a fungal infection and affects exclusively children. The scalp is flaky, showing random patches of hair loss with broken hairs; the appearance of such areas resembles woven lace.
| Figure 7. Cicatricial alopecia seen in lichen planus and discoid lupus erythematosus |
Skin scrapings are taken to identify fungi. Culture takes four to six weeks, so a Wood's lamp examination of the scalp may be helpful. When Microsporum canis (the most common fungal agent) is present, a greenish-blue glow is visible over the affected areas. This allows you to start treatment earlier.
Topical treatment is ineffective for tinea capitis, and a six-week course of griseofulvin is required to control the infection. In severe cases with a pronounced inflammatory component (kerion) due to peeling, permanent hair loss is observed.
| Figure 8. Moderate hairline psoriasis. Scalp psoriasis produces thicker scales than eczema |
Trichotillomania. With this disease, the patient intentionally or unconsciously constantly pulls and twists the hair, which breaks due to this. As a rule, hair problems are not resolved until the underlying mental illness is eliminated. The treatment process can be quite lengthy. During this time, the patient often continues to lose hair. The prognosis is better in children than in adults.
- Scarring alopecia
Cicatricial alopecia is seen in conditions such as lichen planus (LP) or discoid lupus erythematosus, as well as after injury. The scalp is tense to the touch, with patchy areas of alopecia and erythema. It is difficult to restore the skin at the site of the scar, but it is possible to stop the further spread of the disease by treating the blooming edge of the area of active damage with a local steroid in cases of PL or discoid lupus. A biopsy confirms the presence of a scar and often determines the cause of the disease. You should also look for other cutaneous manifestations of PL or discoid lupus erythematosus.
- Peeling skin
This is another common dermatological problem, and flaking can affect just the scalp or be part of a larger skin lesion, as with eczema or psoriasis. The leading symptoms are itching and dandruff - both of which bring significant inconvenience to the patient.
| Figure 9. Severe form of scalp psoriasis. If thick scales form, a cream with 10% urea or olive oil can soften the scales |
Scalp eczema is usually a consequence of seborrheic dermatitis; At the same time, the skin itches and is covered with thin scales. The nasolabial folds, as well as the chest and back are often affected.
Treatment is carried out with local steroid drugs in the form of lotion or mousse, as well as tar or an antifungal shampoo, for example containing ketoconazole. Symptoms may return during stress or illness. When using coloring solutions, contact dermatitis may occur. The diagnosis in most cases follows from the anamnesis; To confirm the diagnosis, the plaque is examined.
With psoriasis of the scalp, the scales are thicker, the peeling is located at the border of hair growth and moves to the forehead or neck. It can be in the form of plaques or cover the entire scalp.
If the scales are not very thick, you can try the same treatment methods as for eczema, or a lotion (ointment) with calcipotriol. However, this is not enough to combat thicker scales. First you need to take measures to reduce the thickness of the scales. To soften and reduce peeling, use a cream with 10% urea or olive oil.
An alternative is coconut oil, a mixture of tar, coconut oil and salicylic acid.
This product stains your hair and has an unpleasant odor, but it is very effective when used regularly. Coconut is applied in the evening and left overnight. The drug stains clothing, so instruct the patient to use an old pillow. As the peeling decreases, you can move on to less unpleasant treatment methods. Further reading 1. Mortimer CH, Rushton H., James KC Effective medical treatment for common baldness in women // Clin. Exp. Dermatol. 1984; 9: 342 – 348. 2. Olsen EA, Weiner MS, Amara LA et al. Five years folloe-up of men with alogenic alopecia treated with topical minoxidil // J. Am. Acad. Dermatol. 1987; 16: 643 – 649. 3. Kligman AM Pathologic dynamics of human hair loss. 1. Telogen effluvium. Arch. Dermatol. 1963; 87: 609 – 611. 4. Simpson NR Alopecia areata. In: Desiases of Hair and Scalp // Eds Rook AJ, Dawber RPR Blackwell Scientific Publications, Oxford 1991: 296 – 333.
Note!
- Hair goes through a cycle of growth (anagen) and loss (telogen); normally, a person loses up to 100 hairs per day. Only when this figure is exceeded does hair loss become noticeable
- Alopecia areata can develop at any age and in both sexes, but teenagers and young adults are more often affected; it may be associated with other autoimmune diseases such as thyroid disease and vitiligo. Most of the nests spontaneously overgrow
- Up to 60% of women over 30 years of age suffer from more or less severe androgenetic alopecia; After menopause, the incidence increases. Like men, hair loss occurs primarily at the front and top of the head. In this case, women should be reassured by saying that such hair loss is rarely severe
- Scalp eczema is usually caused by seborrheic dermatitis and is accompanied by itching. The skin is covered with thin scales. Treatment consists of topical steroids and tar or an antifungal shampoo such as ketoconazole
- Diffuse baldness can occur after pregnancy, serious illness or surgery (telogen effluvium) and can be quite severe.
Hormonal factors
A problem with any endocrine gland can lead to pathological hair loss. Most often this is the thyroid gland (hypo- or hyperfunction, which is very typical for our country, since we are in an endemic zone where there is a lack of iodine), ovaries (the most common cause is polycystic ovary syndrome, disturbances in the production of estradiol, dihydrotestosterone), as well as the adrenal glands (produce cortisol) and the pituitary gland (prolactin). Hair loss often occurs with diabetes, mainly type 1.
In any of these situations, the normal balance of hormones is disrupted, which leads to increased hair loss, impaired restoration, or deterioration of the structure of the hair shaft. In such cases, it is necessary to carry out complex therapy, treatment simultaneously with a trichologist and an endocrinologist, since only normalization of hormonal levels can stop hair loss, but not improve hair growth and structure. This is one of the main mistakes of patients who think that normalizing hormone levels is enough.
Causes of problems
The reasons that can lead to hair problems can be divided into external and internal:
- External – hair dyeing and bleaching, prolonged wearing of tight and uncomfortable hats, tight hairstyles, injuries, improper care, aggressive environmental factors
- Internal - these are various skin diseases, intoxications of the body, infectious diseases, the postoperative period, allergic reactions, hormonal disorders, disorders of the nervous system, deficiency conditions, disruption of the gastrointestinal tract, etc.
Toxic factors
These include the effects of anesthesia during surgical interventions, taking a number of trichotoxic drugs (retinoid group, antibiotics, etc.). A separate risk group is cancer patients undergoing radiation or chemotherapy treatment. It should be noted that in these situations, in most cases, the hair recovers on its own after the cessation of exposure. The criteria for this are the duration of hair loss of no more than 2-3 weeks, slight loss of volume, rapid recovery, hair growth. If this does not happen, then it is better to contact a trichologist.
Symptoms
Normally, a person loses from 25 to 100 hairs per day. If more hair falls out, it is easy to notice when combing and washing your hair. The hair becomes thinner, the parting becomes wider, the frontal hairline shifts, and bald patches appear.
The first noticeable signs of androgenetic alopecia in men are a backward displacement of the frontal hairline (receding hairline) and baldness on the crown of the head; in women, thinning of the hair on the crown, thinning of the hair in the parting area.
The main symptoms of alopecia areata: hair loss in patches in any area, the degree of loss varies and can be total. Hair loss is usually not accompanied by skin symptoms (pain, itching, flaking).
Atypical types of hair loss
The so-called idiopathic alopecia (that is, with an unknown cause) includes focal forms. They are characterized by the formation of areas devoid of hair. There are single, multiple, subtotal, total and universal forms of alopecia. In a one-time, first case, the hairline often recovers on its own without treatment within a year (with the exception of the universal form).
The cicatricial form (Broca's pseudopelade) is also known. In this case, a transplant is indicated; the treatment is ineffective, since the root is replaced by connective tissue, that is, in fact, there is nothing to treat.
Laboratory tests for diffuse effluvium
In patients with effluvium of unknown cause, laboratory testing should be performed to exclude, in particular, the following: Iron deficiency (ferritin) (7) Thyroid dysfunction (TSH, T3, T4) Stage II syphilis (TPPA test). Syphilis is very rare, but omitting an appropriate history or TPPA test in a patient with hair loss can have serious consequences for both the patient and the clinician if neurosyphilis develops further.
Post-COVID hair loss
Recently, the number of patients complaining of very severe hair loss has increased. Very characteristic signs are a flurry of sudden hair loss, which occurs all at once, in one day, and rapid (2-4 weeks) loss of volume 2-3 months after suffering from COVID. Initially, doctors believed that this was a reaction to aggressive therapy, but then patients began to come in who suffered from the disease in a mild form or were completely on their feet. Conclusion: the virus itself has a trichotoxic effect. Treatment with a trichologist is required if hair loss lasts more than 1–2 weeks. The prognosis is usually positive.
Trichologist
Almost every person has a need for a good trichologist at least once in their life, because, unfortunately, there are many factors that negatively affect the condition of our hair and scalp and they surround us all the time.
A trichologist will help you determine the cause and cope with the problem of hair loss and scalp diseases, preventing its reappearance and progression.
A trichologist is a specialist who has undergone primary training in the specialty of dermatovenerology and received additional education in the field of trichology. A trichologist has all the necessary knowledge and skills to diagnose diseases of the scalp and hair, performs various diagnostic procedures, recommends and applies effective methods of treating hair diseases, taking into account individual characteristics and concomitant diseases, and also deals with the prevention of hair loss and scalp diseases.
In our clinic, trichological appointments are conducted by a professional certified trichologist, Marina Nikolaevna Chernova.
Alopecia areata
An autoimmune disease characterized by non-scarring hair loss. It is a widespread pathology - up to 3.8% of all dermatologist patients suffer from focal alopecia. About 20% of patients are children, and in 60% the disease manifests itself before the age of 20 years.
Pathogenesis of alopecia areata
The exact pathogenesis of alopecia areata is unknown. The most popular hypothesis is that it is an autoimmune condition associated with a T-cell immune response in genetically predisposed individuals.
Clinic for alopecia areata
Alopecia areata is usually asymptomatic, but some patients experience burning or itching in the affected area. About 80% of patients have 1 area of baldness, 12.5% have 2 areas, 7.7% have 3 or more areas. Alopecia areata most often affects the scalp - 70–95% of cases, less often the beard - 28%, eyebrows - 3.8% and limbs - 1.3%.
Localized form (alopecia areata) - less than 50% of the hair falls out, the affected areas are limited, in most patients the hair grows back spontaneously within a few months ( Fig. 5 ).
Common form (total/universal alopecia) - more than 50% of hair falls out; this option is less common (on average in 7% of patients). In 30% of patients with total alopecia, complete hair loss occurs within 6 months after the onset of the disease.
Rice . 5. Alopecia areata (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-18-4-1.html
Trichoscopy for alopecia areata
- Short vellus hair
- Yellow dots
- Black dots ( Fig. 6 )
- Broken hair
- crimped hair
- Exclamation mark hair
Rice. 6. Trichoscopic signs of alopecia areata: black spots ( blue arrow ) and crimped hair ( red arrow ) (Jha AK, et al. Dermoscopy of alopecia areata - a retrospective analysis. Dermatol Pract Concept 2017; 7(2): 53–57)
Types of seborrhea
Depending on the location of the lesion, seborrheic dermatitis is distinguished:
- faces;
- scalp;
- widespread (face, scalp, upper back and chest are affected).
Depending on the duration of the disease, the following forms of seborrheic dermatitis are distinguished:
- acute;
- chronic.
At the initial stage, dry seborrheic dermatitis develops. It is characterized by brittle hair and excessive flaking of the skin, which falls off onto clothing in the form of dandruff. At this stage, there is a decrease in the secretory function of the sebaceous glands and the disease is not difficult to cure.
In oily seborrheic dermatitis, the sebaceous glands produce excessive amounts of sebum. Dandruff has a yellowish tint, and red inflammatory lesions form on the skin. Oily dandruff quickly makes hair greasy. This disrupts the protective function of the skin. Layered scales cover the inflamed skin. Pain with oily seborrhea is less pronounced than with dry seborrhea. However, skin irritation causes itching and scratching, which further traumatizes the skin.
If the causes of oily seborrhea are not identified and eliminated, then frequent washing will tidy up the hair for a short time. Under the influence of hyperfunction of the sebaceous glands, skin cells quickly die and form areas of flaking and dandruff.
The wrong choice of skin and hair care products aggravates the course of the disease. As a result, the skin is dry, dehydrated, prone to injury and infection.
With a mixed form of the disease, there are signs of dry and oily seborrhea.