The absence of unpleasant shine, pimples, blackheads or peeling and areas of irritation is the dream of every girl. If the face is far from perfect, discomfort, self-doubt arise, and self-esteem decreases. To live in harmony with yourself and your characteristics, it is not enough to convince yourself that all troubles with the epidermis are age-related and will someday pass. You need proper and complete care for oily, sensitive or dry skin, which will help minimize areas of inflammation and irritation, provide adequate protection from the negative effects of the environment and bring you closer to your ideal.
Unwanted Shine: Why Problems Occur
First, let's talk about skin that is excessively oily: pimples and blackheads constantly appear on it, it has a rough pattern, and is often rough to the touch. Why is this happening? The main reason is the active work of the sebaceous glands.
What caused it?
- Constitutional characteristics (for example, a tendency to diseases of the gastrointestinal tract).
- Hormonal imbalance (most often occurs during puberty and pregnancy).
- Nervous disorders that cause deterioration of the skin.
- Endocrine diseases (directly related to increased production of sex hormones or their deficiency).
- Improper diet (with a predominance of fatty and spicy foods, lack of vitamins).
- Improper care (use of inappropriate cosmetics or complete lack of hygiene and cosmetic procedures).
Lumpy, oily skin that is prone to acne occurs in both women and men. This problem makes itself felt especially often in adolescence. The exacerbation occurs in the summer.
results
Patients with acne-type skin sensitivity (n=5) used the Topicrem Calm+ line for increased skin sensitivity that developed during external or systemic anti-acne therapy. On the 5-7th day of therapy, all patients showed a decrease in the intensity of symptoms, and on the 10-14th day - their complete regression.
Clinical case 1. An 18-year-old female patient complained of a burning sensation, a feeling of skin tightness and redness of the facial skin. Since the age of 16, the patient has been bothered by acne on her face. Burning and redness of the facial skin appeared on the 5th day of using the drug for external treatment of acne (adapalene gel).
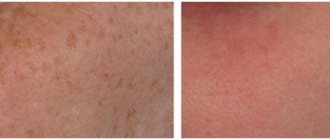
Status localis. On the skin of the face (forehead, cheeks, chin) there are multiple closed comedones, inflammatory papules, single pustules, as well as pink erythema, the location of which coincides with the areas where the therapeutic gel is applied. In the erythema area there is slight peeling of the skin. Diagnosis: acne vulgaris (L.71), simple irritant dermatitis caused by drugs (L.24.4). It is recommended to temporarily cancel external treatment. Medical and cosmetic care was prescribed in the form of monotherapy with Topicrem Calm+ (micellar water, light cream). A significant reduction in symptoms was noted on days 5-7 of treatment (Fig. 2) .
Rice. 2. Acne type (S1) skin sensitivity.
a - before treatment; b — after 7 days of treatment with Topicrem Calm+.
Ten patients with rosacea-type skin sensitivity (mainly with the erythematous-telangiectatic stage), using Topicrem Calm+ products, noted a rapid regression of subjective sensations (on the 2nd day) and a significant decrease in the intensity of skin manifestations by the 7-10th day of therapy.
Clinical case 2. A 45-year-old patient complained of episodes of transient redness of the skin under the influence of emotional and nutritional factors, burning of the skin upon contact with water, and rashes on the skin of the cheeks. Considers himself sick for 1 year. It was not treated independently, the rash periodically regressed spontaneously. Recently, the skin process has become persistent.
Status localis. On the skin of the cheeks there is diffuse erythema of a pale pink color, against which isolated bright pink papules with a diameter of up to 0.3 mm, single finely looped telangiectasias and slight peeling in the cheek area are observed. Diagnosis: rosacea (L.71). Based on your skin type (combination type with increased oiliness in the T-zone), micellar water and Topicrem Calm+ light cream are prescribed. The patient noted the disappearance of subjective sensations in the first days of using the cream. A significant regression of skin rashes was observed on the 7th day of treatment (Fig. 3) . The patient continued to use cosmetics after the end of the observation period.
Rice. 3. Rosacea type (S2) skin sensitivity.
a - before treatment; b — after 7 days of treatment with Topicrem Calm +.
There were 6 patients with S3 type of skin sensitivity under our supervision. Selecting care products for patients with this type of sensitivity is a difficult task. The correct selection of moisturizer texture based on skin type is of fundamental importance. Sometimes the wrong choice of care product causes negative effects.
Clinical case 3. A 35-year-old female patient complains of burning and redness of the skin of the nasolabial folds when applying cosmetic cream, and a feeling of skin tightness after washing. I asked for a selection of facial skin care products. Status localis. There are no rashes on the face, the skin is pale and dull. In the T-zone, enlarged pores, increased greasiness, and oily shine are observed. There is fine peeling on the entire surface of the facial skin. Taking into account the combination skin type, dehydration and hypersensitivity of the skin, therapeutic and cosmetic care using Topicrem Calm+ cosmetics (micellar water and light cream) was prescribed. On the 2nd day of treatment, the patient noted the appearance of rashes on the skin of the forehead (Fig. 4) , increased greasiness in the area of the nasolabial folds and chin. It is recommended to change the form of the cream to a fluid, with the use of which a rapid regression of rashes and the disappearance of subjective complaints were noted. The patient continued cosmetic care using Topicrem Calm+ fluid.
Rice. 4. S3 type of skin sensitivity. Exacerbation after using light cream Topicrem Calm + .
The majority of observed patients (n=19) had type 4 skin sensitivity (S4), prone to contact dermatitis. In all patients, the use of Topicrem Calm+ products was found to be highly effective. Subjective sensations (feeling of tightness, burning) regressed on the 2-3rd day of therapy, clinical manifestations - on the 7-10th day of treatment. By the end of the observation, the appearance of the skin also improved: dullness, even color and freshness of the skin appeared, peeling regressed.
Clinical case 4. A 45-year-old female patient complains of a feeling of tightness and tingling of the skin when exposed to adverse weather conditions and contact with water. The duration of the disease is more than 5 years. Rashes began to appear on my face periodically.
Status localis. The skin of the face is matte, the pores are narrowed. On the skin of the cheeks and temporal areas there are multiple erythematous spots with a diameter of 0.5 to 1 cm, with blurred boundaries. There is slight peeling on the surface of the spots. Diagnosis: simple irritant dermatitis (L.24), weather-dependent (Fig. 5) . Taking into account the dry skin type, the patient was prescribed therapeutic and cosmetic care with Topicrem Calm+ using micellar water and rich cream. A rapid regression of subjective sensations was noted after 1 day. By the 7th day, the symptoms of dermatitis and peeling regressed, and the appearance of the facial skin improved. The patient continued cosmetic care.
Rice. 5. S4 skin sensitivity type.
a - before treatment; b — after 7 days of treatment with Topicrem Calm+.
During the survey, the majority of patients highly rated the products of the Topicrem Calm+ cosmetic line (39 patients when evaluating micellar water and 33 patients when evaluating moisturizer). Only 2 patients gave an unsatisfactory assessment when using a moisturizer (the appearance of “irritation” of the skin, increased oiliness), which is due to the incorrect choice of its texture (Fig. 6) .
Rice. 6. Subjective assessment by patients of the tolerability of cosmetics. Excellent (3 points), good (2 points), unsatisfactory (1 point).
Life without water: dryness and tightness
It’s not just the excessive work of the sebaceous glands that worries many women. A lot of anxiety and discomfort arises due to dehydration of the surface layer of the epidermis. Loss of moisture leads to peeling, redness, and irritation. This problem is the opposite of the one discussed above, but no less relevant.
If oily skin shines, then dry skin looks dull, dead scales appear on it, it suffers from exposure to strong wind or sun, and wrinkles form on it earlier.
The causes of dehydration can be different - both external and internal:
- Genetic predisposition (people with blond hair and pale skin most often experience peeling and irritation).
- Disturbance in sleep patterns (if you don’t get enough rest, this affects the condition of the epidermis).
- Poor nutrition (lack of protein, vitamins B, A, C and E, polyunsaturated fatty acids, a lot of sweets, strong tea and coffee).
- Diseases of the liver and kidneys (in a person suffering from impaired functioning of the kidneys and liver, the elasticity of tissues is lost, the barrier and moisture-saving properties of the epidermis deteriorate).
Lack of proper care can also cause the condition to worsen.
SKIN WITH PIGMENTATION
Skin spots may appear due to the body's overproduction of the pigment melanin, which is produced by the enzyme tyrosinase as a natural defense against exposure to sunlight. Special protective cosmetics with an SPF factor will help prevent their appearance: it weakens the effect of ultraviolet radiation on the skin.
Search in:
Azelaic, lactic, ferrulic, mandelic, kojic, tranexamic, citric acids; Arbutin; Vitamin C; Licorice root extract; Acerola extract; Niacinamide; SPF 30/50;
Sensitivity not to the face: irritation and redness
The last type that I will talk about in this article is sensitive facial skin, which, like dry and oily skin, requires special care. Spots often appear on it, it has an uneven texture, the surface is rough to the touch, and there is often a feeling of tightness and itching.
What is this? Dry skin that has not been properly cared for often transforms into sensitive skin. But there are other reasons:
- Previous rosacea or seborrheic dermatitis.
- Increased nervousness, constant stress, depression.
- Incorrect diet (lack of vitamins and amino acids, predominance of fatty foods).
- Contaminated water used for hygiene procedures.
- Negative environmental impact.
Such skin causes its owners a lot of trouble: irritation can appear on it after washing, applying cosmetics, incorrectly selected skincare procedures, walking under gusts of cold wind or hot rays of the sun. There are many factors influencing the condition of the epidermis. Our main task is to minimize unwanted reactions, restore and strengthen barrier properties.
Next, I will talk about how to prevent the appearance of oily shine, redness, inflammation, dryness, tightness and irritation.
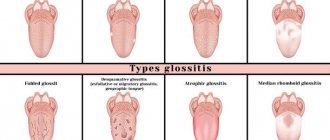
Sensitive Skin Types
Depending on the causes of irritation, skin is divided into several types:
- Weak from birth, most often light and dry. Reacts negatively to any external stimuli. Owners of this type most often cannot spend time in the sun.
- Situationally sensitive - due to improper care, poor-quality cosmetics or aggressive procedure. If you do not address the aggravating factors and take care of your skin, all negative consequences will disappear.
- Sensitive due to internal problems: nervous exhaustion or severe stress, internal diseases. This type needs to be treated together with an endocrinologist.
If you suspect that you have sensitive skin and know how to determine it, all that remains is to choose the right care.
Proper care for oily and problem skin
I’ll start with the most important thing - it must be extremely delicate and careful. Excessive enthusiasm can lead to dryness of the surface layer of the epidermis. All you need is:
- High-quality cleansing is gentle and soft, no matter how rough the relief may seem. I advise you to use hypoallergenic emulsions, foams and gels based on natural ingredients.
- Reducing sebaceous secretion - this task is effectively handled by special cosmetics that regulate the balance between dehydrated and oily areas, mattify and tighten pores.
- Masking imperfections - using products that will not provoke more inflammation and irritation of the skin.
- Effective protection against the negative influence of the environment - preventing the harmful effects of the sun and sources of ultraviolet radiation.
- Sufficient hydration - with the help of serums, creams, tonics and masks that retain moisture in the epidermis.
Oily problem skin needs gentle cleansing. For washing, you should use a variety of foams, emulsions, and gel products based on plant extracts. Cosmetics must be of high quality - I advise you to pay attention to liposomal preparations that deliver active substances directly to the cells of the epidermis. Products you use every day should have an acidic pH.
Please note that the water for washing should not be excessively hot or cold - only at room temperature. Do not use bar soap, which dehydrates the skin. For effective cleansing, you can use exfoliants that perform two functions at once: they promote the gentle exfoliation of dead cells and remove dirt and sebum without damaging the tissue. They should be used no more than 2 times a week.
You need to wash your face 1-2 times a day. For those for whom frequent contact with water is contraindicated due to a decrease in barrier properties, there is a special remedy - gentle emulsions.
You cannot scrub problem skin that is prone to rashes with products containing large abrasive particles - this will lead to tissue damage, inflammation and severe irritation. Frequent classical facial cleansing with intense squeezing is also not recommended - it may leave scars and new pustules may appear.
Lotions based on plant extracts: witch hazel, chamomile, calendula effectively reduce sebum secretion. The effect of glycolic acid relieves inflammation. If acne appears frequently, I advise you to pay attention to pathogenetic drugs that regulate sebum secretion (with extracts of green tea, burdock, cornflower, zinc), have a pronounced soothing effect (with witch hazel, aloe vera, rose extract) and antibacterial effect (with calendula, rosemary, juniper).
Maximum protection from sunlight is also important. Choose products depending on your complexion - the paler you are, the higher the SPF factor should be.
Sensitive skin is a condition characterized by stinging, burning and itching. The diagnosis, pathophysiology and treatment of sensitive skin are still debated. In recent years, studies have been conducted on its epidemiology, indicating a high prevalence and impact on quality of life. The Brazilian population was also considered in these studies. Cosmetics, climate change and disruption of the skin barrier are the main factors that contribute to skin hyperreactivity. New research attempts to bring new knowledge to the topic. This review will describe the epidemiology, triggering factors, pathophysiology, diagnosis and treatment.
Introduction
Sensitive skin is defined as a sensory reaction caused by skin-contacting agents and/or environmental factors, usually without visible clinical manifestation. This condition was first described by Maybach in 1987 under the name Cosmetics Intolerance Syndrome (CIS). In 1990, Fischer calls it "status cosmeticus". A number of publications have shown that this condition can also be caused by environmental factors (cold, heat, sun, pollution, humidity) and therefore the term has been expanded to sensitive skin syndrome (SSS). Possible synonyms for this condition are hypersensitivity, hyperreactivity, sensitivity, intolerance or skin irritation. The sensations described by patients vary widely: itching, burning, tingling, stinging, thickening or dry skin. These symptoms may last from a few minutes to several hours after contact with a cosmetic product/environmental irritant or even due to a cumulative effect after repeated use of the same product. Sensitive skin syndrome can manifest itself in two forms: objective and subjective. Its occurrence is favored by dermatoses that disrupt the protective barrier of the skin, such as atopic dermatitis and acne. In these cases, clinical lesions such as erythema, papules and vesicles may be observed. In the subjective form, the patient experiences only subjective symptoms, without visible dermatitis, and thus the diagnosis is based on the patient's own feelings. The presence of only subjective symptoms in most cases makes it difficult to diagnose this condition, and some authors even believe that the condition has a psychological origin. Using new technologies, it has been demonstrated that there are changes in brain signals in patients with this condition. However, so far it has not been possible to create objective screening tests for diagnosing sensitive skin. Diagnosis, pathophysiology, epidemiology and treatment are still under debate.
Epidemiology
While sensitive skin syndrome has previously been described infrequently, it is not uncommon in current studies. In a study conducted in the UK, symptoms of sensitive skin syndrome were found in 51.4% of women and 38.2% of men. Other European and North American studies have shown similar results. In a European study, Misery et al demonstrated a high population prevalence of the syndrome of 38.4%, indicating the magnitude of the problem. A recent study of the Brazilian population found that 22.3% of men and 45.7% of women consider their skin to be sensitive.
Table 1. Comparison of frequencies of sensitive skin in different countries
| A country | Sensitive skin (%) | Low or insensitive skin (%) |
| Japan | 54,47 | 45,53 |
| Italy | 53,80 | 44,80 |
| France | 51,90 | 48,10 |
| USA | 44,60 | 55,40 |
| Russia | 39,72 | 60,28 |
| Germany | 35,60 | 64,20 |
| Brazil | 34,22 | 65,78 |
| Spain | 31,60 | 68,00 |
| Switzerland | 30,80 | 68,00 |
| Greece | 29,80 | 67,80 |
| Portugal | 27,40 | 72,40 |
| Belgium | 25,80 | 69,80 |
Predisposing factors
Ethnos
Racial differences in skin texture may be associated with symptoms observed in individuals with sensitive skin. Higher sensitivity to capsaicin has been demonstrated in Caucasians, followed by Asians and then blacks. Thin skin is more prone to inflammation due to damage to the skin barrier and increased vascular reactivity. Thus, among white individuals, reports of erythema are more common than among blacks and Asians. However, some authors have found statistically insignificant differences between different ethnic groups.
Floor
According to epidemiological studies, the perception of skin as sensitive in women ranges from 50% to 61%, and in men from 30% to 44%. The syndrome was initially described in women due to their thinner skin than men in addition to hormonal factors that impede skin hydration. However, a 2010 study found sensitive skin in 68% of those surveyed, with no difference between genders. With the increase in the use of cosmetics by men, this condition has also been described in them.
Age
Sensitive skin has been described in patients over 18 years of age, possibly because studies with epidemiological data have primarily included adults. Studies have shown that younger patients have more sensitive skin. On the one hand, older adults have changes in the integrity of skin tissue, which will contribute to sensitive skin. On the other hand, tactile sensitivity decreases with age, and irritability tests are less responsive.
Skin localization.
The main localization is the face, mainly the nasolabial fold. Contributing factors are likely to be greater use of cosmetics in the area, a thinner skin barrier, and the presence of more nerve endings in the face. Other areas of sensitive skin are the flexor surfaces of the forearms, hands, external genital area, and scalp.
Presence of other dermatoses
Atopic dermatitis and other dermatoses such as acne, rosacea, seborrheic dermatitis, contact dermatitis, psoriasis and physical urticaria (dermatographism) are accompanied by a breakdown of the skin barrier or the presence of inflammation. In these patients, sensitive skin is considered an objective form because the dermatosis may present with visible clinical lesions, erythema, cutaneous xerosis, and eczema. In the presence of erythema, the diagnosis of sensitive skin can be mistaken for some dermatoses. However, abnormal sensations, the presence of trigger factors and a short duration of the course indicate a diagnosis of sensitive skin.
Environmental factors
Low temperature, humidity, wind, heat and sunlight favor the development of sensitive skin. Pollution, which is common in the industrialized world, is a contributing factor to the development of the syndrome.
Cosmetic products
Cosmetics are a major factor affecting sensitive skin, especially in women, due to its excessive and inappropriate use. The likelihood of symptoms occurring is increased by the presence of potentially irritating substances in cosmetics (alpha hydroxy acids, propylene glycol, alcohol, fragrances, etc.). Maintaining an optimal skin pH (5.5) maintains the integrity of the skin barrier and adequate skin hydration. When the barrier is damaged, the penetration of substances leads to an inflammatory reaction with the activation of a number of cytokines. Thus, products that alter skin pH favor sensitive skin. Similarly, irritants alter epidermal barrier function to favor sensitive skin, so sensitizing substances phagocytosed by Langerhans cells stimulate keratinocytes and T lymphocytes to produce inflammatory mediators.
Socio-cultural factors
Differences in the prevalence of sensitive skin can be attributed to differences in habits (diet and body hygiene practices) and differences in the perception of symptoms.
Pathophysiology
The pathophysiology of sensitive skin is not fully understood; however, the condition is not thought to have an immunological or allergic origin.
Changes in the stratum corneum
The main hypothesis associated with the appearance of sensitive skin is an increase in the permeability of the stratum corneum, which leads to greater penetration of substances, as well as loss of moisture. There is an inverse relationship between the thickness of the stratum corneum and the permeability of the skin. Reducing the thickness of the stratum corneum facilitates the penetration of substances that can cause the release of cytokines, leukotrienes and prostaglandins. These mediators induce the formation of neurotransmitters, which, in turn, stimulate nerve endings. Transepidermal water loss (TEWL) measurement was used to diagnose sensitive skin. Individuals with elevated TEWL are predisposed to intolerance to products that come into contact with the skin. Thus, adequate skin hydration improves the symptoms of patients with sensitive skin. Studies conducted in menopausal women have shown improvements in sensitive skin with the use of moisturizers and emollients. In addition, decreased levels of ceramides and decreased skin capacity were found in sensitive skin. Dermatoses that result in changes in the permeability of the epidermal barrier, such as atopic dermatitis, seborrheic dermatitis and rosacea, act as predisposing factors for sensitive skin.
Sensory changes
Another evidence, according to the literature, is the presence of dysfunction of the sensory activity of the cutaneous nerves. Current research has demonstrated thermal transient potential receptor V1 (TRPV1) that acts as a stimulator of neurogenic inflammation. Transient receptor potential (TRP) channels are expressed throughout the body in different tissues and with different functions. Both transient receptor potential melastatin 8 (TRPM8) and transient receptor potential ankyrin 1 (TRPA1) are stimulated by cold and certain substances such as menthol. Transport receptor potential vanillide 1 (TRPV1) is stimulated by chemicals, heat, cold, mechanical changes in the lipid layer, and capsaicin; it acts as a cellular sensor that plays an important role in pain and inflammation. In patients with sensitive skin, an increase in sensory impulse is interpreted as an unpleasant sensation. Neurotransmitters and their receptors that regulate the neuroendocrine system of the skin, present in keratinocytes, recognize stimuli and lead to the release of neurotransmitters such as substance P and calcitonin gene-related peptide (CGRP). These neurotransmitters induce vasodilation and degranulation of mast cells, which also act on sensory perception through endothelin A and B (ETA and ETB) receptors. Several published articles have demonstrated the involvement of vanillide 1 (TRPV1) in the induction of rosacea and sensitive skin.
Diagnosis
Clinical diagnosis
Symptoms (burning, itching, tingling, etc.) may or may not be accompanied by signs such as mild erythema, telangiectasia, xerosis, desquamation or urticaria. However, in most cases there are only subjective symptoms. Patients with cosmetic intolerance usually have multiple subjective symptoms, and therefore a careful history taking and evaluation is fundamental.
History and physical examination
It is essential to collect personal, family and professional history, as well as information about habits and use of cosmetic products. A complete physical examination should exclude signs of inflammation and the presence of other dermatosis, such as contact and atopic dermatitis. Due to the frequent lack of objective clinical signs, self-report questionnaires are useful tools for identifying people with sensitive skin. A possible proposed questionnaire is shown in Table 2.
Table No. 2. Questionnaire to identify patients with sensitive skin.
| 1. Do you have increased sensitivity of your facial skin? |
| 2. Do you think that you have sensitive facial skin prone to irritation? |
| 3. Is your skin accompanied by irritation, burning or itching, with or without redness? |
| 4. Do you avoid certain cosmetics that you think may irritate your facial skin? |
| 5. Does your skin experience irritation, burning or itching, with or without redness, when in contact with cosmetics and/or toiletries? |
| 6. Does your facial skin experience irritation, burning or itching after using any cosmetics and/or toiletries? |
| 7. Have you had any adverse reactions on your face when using cosmetics and/or toiletries? |
| 8. Does the expression “cannot tolerate cold weather or cold environments” apply to your facial skin? |
| 9. Does the expression “cannot tolerate hot weather or high ambient temperatures” apply to the skin of your face? |
| 10. Does the expression “cannot tolerate sudden changes in temperature” apply to the skin of your face (for example, when leaving a warm room into a cold room) |
| 11. Do you experience irritation, burning, or itching on your facial skin when exposed to the wind? |
| 12. Do you experience irritation, burning, or itching on your facial skin when exposed to the sun? |
| 13. Do you experience irritation, burning, or itching on your facial skin when it gets dirty? |
Interpretation of the Sensitive Skin Questionnaire. Patients who meet one of the following criteria qualify for sensitive skin:
- Positive answer to 2 questions from questions No. 1-3 - sensitive, reactive and irritated skin;
- Positive answer to 3 questions from questions No. 4-7 - reaction to cosmetics;
- A positive answer to 3 questions from questions No. 8-13 - reaction to the environment.
Additional tests
Although research is being conducted, attempts to develop diagnostic tests to objectively identify the entire sensitive skin profile have not yet been successful, likely due to the heterogeneity of symptoms, the subjectivity of discomfort reactions, and the lack of visible signs. Studies to identify active substances in sensitive skin focus on inflammatory mechanisms such as vasodilation, edema, mast cell degranulation and TNF-alpha release. Some models use neural cell cultures to evaluate inhibition of capsaicin-induced CGRP peptide release by neurons. Clinical studies use the irritation test and TEWL to assess the epidermal barrier. The assessment of sensitive skin remains challenging, however several tests have been proposed to improve the diagnosis of sensitive skin:
1. Sensory reactivity test
This is a cutaneous sensory assessment of the application of chemicals or physical stimuli. The irritation test involves applying 10% lactic acid to the nasolabial fold and saline as a control, followed by rating the intensity of symptoms reported by the patient according to a visual analogue scale. Other substances such as capsaicin, ethanol, sorbic acid and others can be used.
A patient-reported discomfort scale may be used:
- 0: no discomfort or very slight discomfort
- 1: mild discomfort
- 2: moderate discomfort
- 3: severe discomfort
These tests are quick and easy to perform, although they are subjective and have no predictive value.
2. Magnetic resonance
New studies aimed to evaluate brain activation during provocative tests of cutaneous sensory reactivity using nuclear magnetic resonance in both people with normal skin and people with sensitive skin, by testing for differences between the two groups.
3. Irritation tests
These tests measure signs of skin irritation following the application of substances known to be irritants (eg sodium lauryl sulfate), for example using colorimetry or electrical capacitance measurements. These are non-invasive and objective tests. However, they require certain devices.
4. Epidermal functional tests
Epidermal function tests aim to measure structural or physiological changes in the skin following the application of irritants. The most commonly used parameters: measurement of transepidermal water loss, skin pH, epidermal thickness.
5. Dermatoscopy
Recently, some authors have reported the presence of structural changes in sensitive skin visualized by dermatoscopy demonstrating capillary dilatation and confocal microscopy showing thinning of the epidermis.
6. Contact tests
Contact studies and contact phototests should always be considered when evaluating a patient with sensitive skin to rule out allergic and photoallergic contact dermatitis. In addition to sensitivity to standard and additional allergens (according to medical history), it is important to check sensitivity to cosmetic products used by the patient. Unlike patients with allergic contact dermatitis, most patients with sensitive skin react negatively to contact tests.
7. Other methodologies
One way to exacerbate local conditions by increasing the irritant component of product use would be a test in which the test substance is applied to a person's popliteal fossa.
Treatment
Treatment of sensitive skin consists of several stages. In cases where there is a predisposing dermatitis to the symptoms, disease control will improve the condition. During the acute phase, some active ingredients may be used to relieve symptoms, such as mild to moderate potency topical corticosteroids (used for a short period of 3 to 4 days) and topical immunomodulators such as pimecrolimus or tacrolimus (these may be given for a longer period ). In addition, the use of all cosmetics should be discontinued for 2 weeks. After this period, the products are reintroduced one at a time. Before re-introducing the product, it is necessary to carry out a patch test for sensitivity. Proper skin hydration helps restore and maintain the skin's protective barrier. Moisturizers with few ingredients, no fragrance, and no substances that can irritate the skin (such as urea) are indicated. In patients with sensitive skin, photoprotectors should also be used, since, as already mentioned, ultraviolet radiation can also cause symptoms. When it comes to choosing topical products for sensitive skin, you should consider the form of the product and its components. In addition to established tests to assess irritability and sensitivity to foods, you should:
- Assess the stability of components;
- Avoid unnecessary ingredients;
- Leave a few active ingredients (minimal or unique for each product);
- Avoid allergens and common irritants in the composition. When this is not possible, reduce the concentration of these substances;
- Avoid substances that increase the penetration of other substances into the skin, such as ethanol or propylene glycol;
- Give preference to powder cosmetics rather than creams or lotions;
- Use cosmetics that can be easily removed with water;
- Do not use scented products.
Studying the functions of transient receptor potential (TRP) channels, especially TRPV1, has led scientists to discover new perspectives for the treatment of pain. TRPV1 plays an important role in the symptoms of sensitive skin. Trans-4-tert-butylcyclohexanol was identified as a selective inhibitor of TRPV1, antagonizing capsaicin-induced activation. Some protocols are already using antagonists of this receptor as a new line of treatment for sensitive skin symptoms. Another drug described as a TRPV1 inhibitor is furocoumarin, which has properties that reduce pain associated with this receptor. However, a number of experimental studies in which these drugs have been used as a therapy for sensitive skin are still not supported by clinical trials. The demonstration of sensorineural changes by magnetic resonance imaging in previous studies in patients with sensitive skin suggests that it is not only a subjective disease, but also a dermatosis with varied symptoms and several clinical manifestations. The evolution of research into this dermatosis will lead to new treatments and recommendations for patients with sensitive skin in the future.
Care for dry problem skin
There are two essential steps to keep in mind:
- Cleansing
It should be carried out using gentle products designed specifically for skin prone to flaking, dryness and tightness. I recommend gentle foams and soft emulsions.
- Hydration and nutrition
Special lotions, sprays, light creams with antioxidants, oils and hyaluronic acid - one of the most effective means to combat dehydration.
Cosmetics for dry skin should combine soothing and nourishing ingredients. I advise you to pay attention to preparations with natural oils and extracts of medicinal herbs.
If you are concerned about the feeling of tightness and flaking, do not forget that chlorinated tap water can harm you. When washing your face, use water that has previously been passed through a filter. To avoid over-drying after hygiene procedures, wipe your face with a mild toner that does not contain alcohol.
The most favorable period for those with dry skin is summer. On warm days, painful sensitivity disappears or appears extremely rarely. In hot weather, the ideal remedy is a spray with a light formula that evenly covers the face and promotes intense hydration. In winter, additional nutrition is needed. Before going outside, you should apply a special rich cream with a high protection factor.
Care for sensitive problem skin
To avoid irritation and redness, you need to remember one simple rule - no aggressive influence. Only careful care is allowed.
- Eliminate irritating components
These include alkali, anionic surfactants, as well as acids and some oils.
- Avoid overly greasy creams
They have a warming effect, which leads to vasodilation and redness.
- Use only gentle peelings
Mechanical impact is excluded, as is the use of scrubs. The most effective is the use of special exfoliants that do not injure the skin. During the day you should take care of nutrition, at night - about strengthening barrier properties and recovery. Choose professional hypoallergenic cosmetics that will not only protect against irritation, but also remove redness, increase firmness and elasticity.
If you are hypersensitive, washing with soap is contraindicated. Use special soft products - foams, gels or emulsions. Do not forget that frequent changes of medications will not help you, but will only worsen the condition of the epidermis. So the best option is to use products from one company or series.
Choosing cosmetics for problem skin is a particularly difficult task. I advise you to stick to liposomal products. They have passed clinical tests, are hypoallergenic, and contain natural ingredients that eliminate the cause of defects and do not cause harm. A professional approach helped us find unique formulas for each case – even the most complex ones.
| Problem | Solution | Means |
| Increased sebum secretion and redness | Salicylic acid eliminates excess sebum, lime extract launches regeneration processes, and aloe moisturizes and gently relieves inflammation. | Pro Quick ViewSOS cleansing mask, 50 g1 290 ₽ Add to cart Checkout |
| Dryness and flaking | Lavender oil promotes intense hydration, while witch hazel gently cleanses, tones and eliminates flaking. | |
| Increased sensitivity | Rose extract soothes the skin, relieves irritation and softens dry areas. | Pro Quick view 350 ml |
Cosmetics for oily skin
Cosmetics for oily skin care should contain:
- herbal ingredients (chamomile, witch hazel, lemon balm, sage, rosemary, quince bark, ylang-ylang),
- alpha hydroxy acids (fruit acids),
- urea,
- silicon,
- ammonium compounds,
- vitamins A and E,
- bisabolol,
- azulene and aluminum salts.
The use of natural mineral cosmetics will solve the problem of “blackheads”. It has antibacterial properties and protects the skin from UV radiation. An alternative to foundation can be concealer, which, when applied topically, masks skin imperfections. Zinc oxide in concealer will be an advantage.