Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
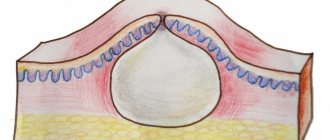
Melasma (chloasma, pregnancy mask, melasma, melasma , chloasma ) is a chronic recurrent acquired dyschromia caused by increased activity of epidermal-melanin units. The epidermal-melanin unit is a union that consists of one melanocyte and several keratinocytes, facilitating the transfer of pigment granules from the melanocyte to the surrounding keratinocytes.
In our company you can purchase the following equipment for the treatment of melasma:
- M22 (Lumenis)
- Fraxel (Solta Medical)
Melasma occurs in areas of the skin that are exposed to severe and/or regular sun exposure, more often in women of reproductive age. It negatively affects quality of life due to its high prevalence, involvement of visible areas of the face and body in young patients, and relative resistance to therapy. Melasma affects mainly women (90% of cases) of any race, but more often with dark skin phototypes (IV-VI). The average prevalence of the disease in the population ranges from 8.8% to 40%. According to some reports, the likelihood of melasma developing during pregnancy is 15–50%.
Chloasma is the name given to melasma that occurs during pregnancy (“mask of pregnancy”). The word chloasma comes from the Greek chloazein (green), while melasma comes from the Greek melas (black). Since chloasma is never green, it is more correct to call it melasma.
What are melasma and chloasma
Melasma is a benign skin pigmentation with increased deposition of melanin pigment in cells.
Often the concepts of melasma and chloasma are confused or considered synonymous with non-cancerous pigmentation. However, the most common difference is the following:
- Melasma is the general name for benign skin hyperpigmentation
- Chloasma is pigmentation that occurs during pregnancy, i.e. essentially one of the manifestations of melasma that arose for a specific reason.
This classification is the most common and recognized among European and American specialists.
Etiology and pathogenesis
An important etiological factor for melasma is heredity . In one study of 324 women with the condition, 48% reported having it in their immediate family. Melasma almost always occurs in identical twins, while it may not occur in fraternal siblings.
Another factor in the appearance of melasma is ultraviolet radiation of spectrum B (UVB, 290–320 nm) and spectrum A (UVA, 320–700 nm). It causes lipid peroxidation, promoting an increase in the number of reactive oxygen species, which stimulate melanocytes to actively synthesize pigment.
Melasma is caused by hormonal changes in the body. Moreover, this can be not only pregnancy, but also taking oral contraceptives. In nulliparous women, there is usually no significant increase in estrogen or melanocyte-stimulating hormone (MSH) levels, but they do have an increase in the number of cellular estrogen receptors in the area of melasma lesions. In postmenopause, melasma can occur while taking drugs with progesterone (whereas it usually does not occur when estrogen is prescribed), which indicates a significant role of this hormone in the pathogenesis of the disease.
In general, the pathogenesis of melasma has not been well studied. It is noted that in this case, melanogenesis differs from tanning and post-inflammatory hyperpigmentation. In this case, epidermal-melanin units, mast cells and cytokines produced by fibroblasts and endothelium are involved in the process. Abnormalities that differ from other acquired pigmentation disorders occur in the upper layers of the dermis.
Why does melasma occur?
It is believed that the occurrence of melasma is based on a genetic predisposition , and the process of excessive formation of pigment in cells is triggered under the influence of a number of predisposing factors:
- Excessive ultraviolet exposure (approximately 50% of cases). Prolonged exposure to the sun, as well as visiting a solarium.
- Hormonal imbalance , acute and chronic inflammation of the reproductive system, reproductive organs (endometriosis),
- hormonal contraceptives (accounts for 30%);
- Hormonal disorders : dysfunction of the ovaries, thyroid gland, hormone replacement therapy and other conditions that change the hormonal background of a woman and contribute to the appearance of age spots.
- Pregnancy - 18% of cases: changes in estrogen and progesterone levels.
- Taking medications : some groups of antibiotics and photosensitizers.
- Diseases of the gastrointestinal tract and digestive organs : liver, pancreas.
According to modern authors, the predisposing factors of pathological pigment formation are: in 52–63% of cases, excessive ultraviolet radiation, in 25–32% — hormonal disorders not associated with pregnancy or inflammatory processes, and in 18–24% — pregnancy.
It has been established that the process is triggered by exposure to UV rays and a sharp increase in the number of free radicals occurs. Free radicals trigger fat oxidation, which leads to DNA damage in melanocytes. In addition, UV rays themselves damage the DNA of cells. Result: pigment cells melanocytes increase the production of melanin and redistribute it along the processes into the cells of the epidermis.
You can find out how to deal with pigmentation in this article .
Clinical manifestations
The disease manifests itself either as a single lesion or as multiple foci of dark brown or black hyperpigmentation, symmetrically located on the face and/or neck ( Fig. 1 ). Clinically, there are 3 variants of melasma localization:
- Centrofacial (forehead, cheeks, nose, upper lip and chin)
- Painting (nose and cheeks)
- Mandibular (in the lower jaw area)
It is still unclear why some areas of the face may remain intact with melasma. This is thought to be related to the density of the sebaceous glands on the skin and their activity. In rare cases, melasma appears clinically on the forearm and is associated with progesterone use.
The depth of pigment in melasma can be determined using a Wood's lamp - this method is good for determining epidermal melanin, but poorly assesses the dermis. One can only indirectly judge the presence of melanin in the dermis with a bluish tint of hyperpigmentation in the glow of a Wood's lamp. Unfortunately, this approach does not work for people with dark skin phototypes.
Clinicians typically use the Melasma Area and Severity Index (MASI) and the Melasma Quality of Life scale (MELASQoL) to assess disease severity.
Rice . 1. Centrofacial melasma (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-161.html
Preventive measures for the appearance of chloasma
Experts have developed a set of measures, the observance of which allows both to prevent the appearance of chloasma and to get rid of existing spots on the skin:
- You should take hormonal contraceptives with caution, or completely stop using them and replace them with other types.
- Use cosmetics that contain protection against the harmful effects of ultraviolet rays.
- Cleanse the skin only with delicate products and moisturize it regularly.
- Avoid dietary supplements, food products, and medications containing photo-sensitizing substances.
- Any cosmetic whitening procedures are used only after consultation with a specialist to avoid relapse.
How to eliminate chloasma with peeling is shown in this video:
Chloasma should be treated by doctors and professional cosmetologists. A good result comes from a comprehensive solution to the problem, eliminating the cause from the inside and outside.
Principles of treatment
Hyperpigmentation with melasma appears slowly and disappears just as slowly with treatment, so doctors and patients should be patient.
An important therapeutic factor is complete avoidance of sunlight . Moreover, sunscreen cosmetics cannot fully protect the skin, since they usually block only the UVB range, while UVA gets on the skin and continues to worsen the condition of the disease. Therefore, if you have melasma, it is recommended to wear closed clothes, hats with wide brims and visors, and stay mostly in the shade. This does not replace the need for UV filters, although patients should note that they should not be relied upon solely.
Hydroquinone is used as a skin lightening ingredient in a number of countries where it is permitted . To increase effectiveness, it is combined with tretinoin and/or glycolic acid (due to their exfoliating effect, they improve the penetration of hydroquinone) and corticosteroids (to reduce inflammation). In one study, a formulation containing 4% hydroquinone, 0.15% retinol and antioxidants significantly reduced melasma pigmentation after 12 weeks of use. It is important to remember that because hydroquinone penetrates the skin well and can be absorbed into the blood, it should not be used during pregnancy or breastfeeding. In addition, it has a number of serious side effects, which is why it has been banned in the European Union and Switzerland since February 2001.
Tranexamic acid acts in several directions at once: it directly blocks the formation of melanin in cells, does not allow it to accumulate locally, and disperses the melanin that is already present in the skin. In cases where it is necessary to act on deeper-lying pigment granules, tranexamic acid is transported into the dermis using liposomal delivery systems.
Azelaic acid can be used to treat melasma in the form of a 15% gel or 20% cream.
It is impossible not to note the possibilities of chemical peels - glycolic acid (50–70%, pH 2.0–3.0), trichloroacetic acid 10–30%, Jessner’s solution (14% lactic acid + 14% salicylic acid + 14% resorcinol) are recommended. , resorcinol (20–50%).
Long-term improvement in refractory melasma has been reported following microneedling , a minimally invasive procedure in which the skin is pierced with short, thin needles, resulting in stimulation of fibroblast proliferation, release of growth factors, and increased collagen production. However, the exact mechanism for the positive effect of this procedure on melasma has not been established.
To treat melasma, such types of hardware cosmetology as non-ablative fractional photothermolysis, IPL therapy and short-pulse Q-switched Nd:YAG laser are used. The principle of operation of fractional lasers is the destruction of micro-areas of the epidermis and dermis, followed by their healing and the formation of healthy, defect-free skin. Thus, the non-ablative fractional laser Fraxel has shown high efficiency in the treatment of melasma when performing 2-3 procedures with an interval of 1 month. Non-ablative fractional photothermolysis is the method of choice for patients with skin phototype IV and above who cannot undergo other laser procedures.
IPL therapy is also actively used to treat melasma . In this case, the target for exposure to high-intensity pulsed light is melanin. This method gives good results in patients with light phototypes. Finally, in cases of difficult-to-treat melasma, the development of which is stimulated by thermal procedures, Nd:YAG Q-switched laser , which also selectively affects melanin, but does not heat the skin, due to its ultra-short pulse duration.
Questions from our users:
- melasma laser treatment
- melasma cream
- melasma effective treatment
- melasma treatment on face
How to get rid of chloasma at home
Alternative medicine recipes cannot be excluded from the arsenal to combat unpleasant cosmetic defects from chloasma.
There are a lot of products prepared using natural ingredients at home, among which you can easily choose the one that suits each individual individually.
- Whitening mask based on cucumber.
For normal and combination skin: take freshly squeezed cucumber juice, soak a napkin in it and place it on the spots. The frequency of the procedure is 3 times for 10 minutes a day. The mask is used daily until the desired effect appears. After this, it is necessary to carry out maintenance procedures 2 times every 14 days. For dry skin: cucumber pulp is mixed with nourishing cream in a ratio of 2 to 1 and applied to problem areas for 20 minutes. Use daily until the desired effect appears.
- Lemon mask: crush one lemon, pour in 100 ml of vodka, leave for 10 days. Cotton wool or a napkin is moistened in the solution and applied to the stains for 20 minutes. Repeat daily until results appear. There is no need to wash off the mask.
- Yeast perhydrol mask is made from 0.5 g of dry yeast, 10 g of 3% hydrogen peroxide and 5 g of ammonia.
- Mix 1 tbsp. spoon of lemon juice, 1 tbsp. a spoonful of vinegar, 2 teaspoons of boiled water. The resulting mixture is applied to the face as a mask or used as a toner.
- A watermelon mask made from the pulp of the berry is applied to the face for 15 minutes. If the skin is too dry, pre-wipe it with olive oil.
- Moisten a napkin with freshly squeezed juice from viburnum fruits and apply to problem areas for 20 minutes. The number of times of use depends on the desired effect.
- A mask of crushed pumpkin seeds (raw), water and honey is mixed to a paste and applied to the spots daily for 30 minutes until the desired result is obtained.
- Sour cabbage has also long been known for its bleaching properties. Soak a cloth with its juice and leave it on the face for 10 minutes. The procedure is done 3 times a day until the brightening effect appears.
Recommendations for using bleaching products
Any drug with a whitening effect causes injury to the skin through mechanical or chemical action. Each drug should be used only after consultation with a specialist.
The selection of the product is carried out solely on the degree of manifestation of the disease and on the type of skin, as well as on individual intolerance to the components. Thus, some preparations contain mercury as a bleaching component.
The reaction to its tolerance by the body should be carried out on the skin of the elbow. If redness or burning occurs, use of the product on the face is prohibited.
For dry and sensitive skin, to get rid of chloasma, you need to use products with a moisturizing base.
Diagnostics
To diagnose chloasma, you need to make an appointment with a dermatologist.
During the examination, the doctor will prescribe the necessary examinations and studies to determine the type and stage of the disease. You may need to consult a gastroenterologist, gynecologist, neurologist and sometimes a psychologist. The following examinations should be carried out:
- coprogram;
- analysis for dysbacteriosis;
- gastroscopy;
- ultrasound examination of the peritoneum and liver;
- biochemical liver test.
Review
The first time I developed chloasma was about 5 years ago after a strong passion for tanning. Then it intensified during pregnancy, and after childbirth it remained the same. I tried a huge number of ointments and creams, folk remedies. There was a noticeable improvement, but after a while the spots darkened again.
So I suffered until a friend recommended a good dermatocosmetologist. He selected me a medicinal cream with kojic acid, lemon and cucumber extracts “MICROCELLULAIRE” and prescribed vitamins B and C. I also had a medium peeling with glycolic acid, 3 procedures.
There are several barely noticeable spots left on the face that are easily hidden under foundation. Now I always use sunscreen and plan to undergo peeling procedures once a year.
Albina Voevodina, 38 years old.
How to remove chloasma on the face
Successful treatment of chloasma is possible after an accurate diagnosis of the diseases that caused it. Once metabolism and hormonal balance are restored, pigmentation of areas of the skin becomes a cosmetic problem that can be easily corrected. For successful recovery you need to follow several rules:
- avoid being in bright sun;
- use sunscreen;
- take vitamins prescribed by the doctor: aevit, folic acid, methionine, riboflavin, injections of B vitamins.
- stop visiting the solarium;
- Avoid using essential oils in cosmetics; they increase sensitivity to the sun and cause pigmentation.
Methods of cosmetic facial correction
A visit to a cosmetologist gives lasting results in the treatment of hyperpigmentation on the face. The work of a cosmetologist on chloasma comes down to the following actions:
- Protection from direct sun exposure. For this purpose, suitable protective equipment is selected for the patient.
- Removing the layer of dead cells. Thus, some of the dark cells are mechanically removed and the spots become lighter. The skin begins to renew itself more actively, and the stain gradually disappears.
- Suppression of melanin production in certain areas. For this, whitening cosmetics with traditional and modern components are used: acids, plant extracts, omega-3 and others.
In addition to cosmetics, hardware procedures are used for correction: dermabrasion, laser corrections, massages, injections.
Medicines
Drugs prescribed for the treatment of chloasma require careful adherence to instructions, dosages and specialist supervision. Overdosing or increasing the time of procedures can lead to the opposite effect: the skin in the affected area will be excessively whitened, and this area will also stand out on the face. In addition, in some cases, actively targeting melasma can cause increased melanin production, causing the spot to darken even more.
To control the production of melanin, doctors prescribe vitamins that affect its production and excretion:
- The essential amino acid methionine effectively lightens chloasma. It is prescribed three times a day, 0.5 g.
- Ascorbic acid, when applied to the skin, easily penetrates the external barrier, stops the formation of melanin, promotes active collagen production and whitens the skin. To enhance the effect, ascorbic acid is prescribed for oral administration.
- Folic acid (vitamin B9) has a beneficial effect on the skin. Among its many beneficial properties is the ability to create invisible protection against UV radiation. Take 0.1 g per day.
- Skinoren cream not only solves the problem of excess pigmentation, it cleanses the skin of inflammation and helps remove traces of acne. The active ingredient of the cream is azelaic acid. It suppresses the development of excess melanocytes, making them non-viable. To get rid of pigmentation, a course of about three months is required. A 2.5 cm strip of cream is enough to apply to the entire face.
Which doctors should I contact for this problem?
Skin problems are dealt with by specialists - dermatologists. You can also start treatment by making an appointment with a therapist, who will write a referral to a dermatologist and specialists in major chronic diseases. Based on the test results and taking into account your medical history, you can receive a referral to a gastroenterologist, gynecologist, oncologist, neurologist and other specialized specialists.
Chloasma during pregnancy
Pigmentation increases during pregnancy; this is a normal phenomenon that should not be dealt with. The areolas and the line at the bottom of the abdomen darken, and freckles become more noticeable. Hormonal changes in the body working with double load provoke the appearance of melasma.
It is advisable for pregnant women to protect themselves from the sun, take vitamins on time, and consider a diet rich in sea fish, herbs, vegetables and fruits.
If spots do appear, they will disappear on their own 3-5 months after birth. If they do not go away, you should consult a doctor. Pigmentation can signal internal problems in the body; after pregnancy, it is especially important to check the proper functioning of the ovaries and thyroid gland; the functioning of these organs may change during pregnancy.
What dermatological processes are chloasma differentiated from?
At an appointment with a dermatologist, the doctor conducts an examination; it is important to clarify the medical history to exclude the congenital or post-inflammatory nature of chloasma.
To select a treatment method for chloasma, dermatoscopy and siascopy are used.
When chloasma appears, the patient is referred for consultation to a gastroenterologist; women are also referred to a gynecologist to identify the possible cause of the appearance of the pigment spot.
Differential diagnosis of chloasma is carried out with:
- borderline pigmented nevus;
- secondary hyperpigmentation;
- melasma of an occupational nature;
- Mongolian spot;
- with large chloasma - with a giant pigmented nevus.
When melanocytes become enemies: basic approaches to the treatment of hyperpigmentation