Dermatovenerologist
Khasanova
Alina Rashidovna
9 years experience
Make an appointment
Pyoderma is the collective name for various purulent-inflammatory skin diseases that are caused by staphylococci, pyococci and streptococci. These diseases can be primary (that is, independent) and secondary - accompanying other diseases. Purulent skin lesions of one kind or another account for a third of all skin diseases. If they occur superficially, then after recovery they can disappear without a trace. When deep layers of skin are affected, there is a risk of scarring, dark areas and other defects.
Causes of the disease
The pathological condition of the organ is caused by bacteria - staphylococcus, streptococcus, pneumococcus, Escherichia coli and Pseudomonas aeruginosa and other microorganisms. They produce waste products - toxins, enzymes and other biologically active substances that irritate the skin and cause an unpleasant reaction - redness, exfoliation (peeling, peeling), swelling and compaction.
In addition to skin disorders, the disease also originates in natural pores - hair follicles, in the openings of the sweat and sebaceous glands.
External factors
The likelihood of the occurrence of the disease increases when the integrity of the skin is violated - ordinary and microtraumas, maceration of the skin.
External risk factors also include overheating or hypothermia of the body, increased sweating, contamination or alkalization of the skin, excessive or, on the contrary, insufficient hygiene. For example, overuse of antibacterial products destroys the natural protective barrier and beneficial bacteria living on the skin. Without protection, the cover becomes dry, cracks appear, and dysbiosis develops - this makes it easier for harmful bacteria to penetrate inside and cause inflammation.
Internal factors
The general condition of the body and immunity also affect the likelihood of pyoderma. Thus, the risk of developing the disease increases in the presence of endocrine diseases (for example, diabetes), obesity, diseases of the digestive or circulatory system, and severe somatic diseases.
Vitamin deficiency, reduced immunity, chronic intoxication, and hormonal disorders also serve as a favorable background for the development of pyoderma. In childhood, the risk of developing the disease is higher due to the structural features of children's skin and the functioning of the immune system.
If there are similar infections (for example, staphylococcal) in other organs, the likelihood of pyoderma caused by the same bacterium also increases.
Are there any complications?
If the immune system is weak and the body is not provided with professional support, the disease will develop and there are risks of complications. In this case, these are inflammation of the lymph nodes, abscesses, scars, sepsis, meningitis, inflammation of internal organs and even thrombosis of cerebral vessels. That is, theoretically, things could lead to complications that would be dangerous not only to health, but also to human life. So the symptoms of pyoderma should never be ignored. This is not just an aesthetic problem. Moreover, against the background of the aesthetic factor, severe psychological conditions can develop, even depression - so this point also cannot be ignored.
Symptoms of pyoderma
The manifestations of pyoderma depend on the causative agent of the disease and the affected area, which makes it difficult to identify a clear list of symptoms. However, if the following symptoms appear, pyoderma may be suspected and it is recommended to consult a doctor:
- inflammation of the hair follicles;
- inflammation of the sebaceous glands;
- the appearance of bubbles with liquid.
We recommend that you consult a dermatologist if any unpleasant, incomprehensible symptoms or manifestations appear on the skin.
Types of pyoderma
Medicine divides pyoderma into superficial, milder ones that are treated by dermatologists, and deep, requiring surgical intervention.
Superficial pyoderma
- impetigo - the sudden appearance of watery blisters that turn into yellowish crusts and bother the patient with severe itching;
- sycosis is a chronic inflammation of the hair follicles of the face - the mustache and beard. Prone to relapse. It is manifested by the appearance of small pustules in the mouth and chin. Over time, the number of inflammatory elements increases, crusts and a purulent infiltrate appear. Sycosis is difficult to treat, with relapses;
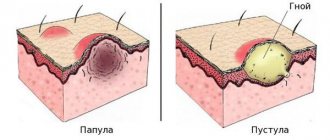
- Ostiofolliculitis is an inflammation of the upper part of the hair follicle. Redness and a 2-3 mm nodule appear in the middle of the follicle, which dries out over time;
- folliculitis is a deeper inflammation of the hair follicle. The affected follicle turns red, swells, and an abscess appears.
Deep pyoderma
- hidradenitis – inflammation of the sweat glands. It occurs not only in the armpits, but also in the groin, labia, and perianal area. With hidradenitis, a large, painful abscess forms;
- A boil is a common inflammation of the hair follicle. It begins with ostiofolliculitis, but the nodule is painful from the very beginning. A purulent melting of the follicle itself and adjacent tissues occurs, the inflammation swells and forms an abscess the size of a walnut. After opening, the dead follicle comes out along with pus. Boils usually leave scars;
- The carbuncle arises from the boil, but spreads more strongly to nearby tissues. Cellulitis (inflammation of cellular spaces) penetrates into the deep layers, affecting the subcutaneous fatty tissue, and sometimes even the muscle membranes (fascia) and the muscles themselves.
A number of pyodermas occur only in children and are not observed in adult patients:
- multiple abscesses - inflammation of the sweat glands of infants;
- ostioporitis - inflammation of the excretory flows of the sweat glands;
- Staphylococcal scalded skin syndrome is a type of severe pyodermatitis caused by staphylococcus. In this case, large blisters appear on the child’s skin, similar to 2nd degree burns;
- epidemic pemphigus (pemphigus) - the appearance of blisters on the skin of newborns. A very contagious disease for children.
Make an appointment
Classification
The main microorganisms that cause pyoderma are streptococcus (Streptococcus pyogenes) and staphylococcus (Staphylococcus aureus). The percentage of diseases caused by other microflora (pseudomonas or Escherichia coli, pseudomonas infection, pneumococci, etc.) is very small.
Therefore, the main classification according to the nature of the pathogen is divided into:
- staphyloderma - purulent inflammation;
- streptoderma - serous inflammation;
- strepto-staphyloderma - purulent-serous inflammation.
In addition, any pyoderma differs in its mechanism of occurrence:
- primary - manifested on healthy skin;
- secondary - which has become a complication of other diseases (most often accompanied by itching).
In addition, pyoderma is divided according to the depth of infection. Therefore, the general classification of pyoderma looks like this:
- with superficial depth of infection (streptococcal impetigo, syphilide-like impetigo, bullous impetigo, intertriginous impetigo (slit-shaped), annular impetigo, streptococcal impetigo, superficial panaritium, dry streptoderma);
- with deep penetration (acute streptococcal cellulitis, vulgar ecthyma).
Staphyloderma includes:
- with superficial depth of infection (superficial folliculitis, ostiofolliculitis, acne vulgaris, sycosis vulgaris, epidemic pemphigus of newborns);
- with deep penetration (deep folliculitis, furuncle, furunculosis, carbuncle, hidradenitis).
Strepto-staphyloderma includes:
- with superficial depth of infection (impetigo vulgar);
- with deep penetration (chronic ulcerative pyoderma, chancriform pyoderma).
Diagnosis of pyoderma
The reason for testing for pyoderma is the appearance of inflammatory elements on the patient’s skin. The doctor’s task is to establish the exact type of disease and its severity.
For this purpose, bacteriological examination of the contents of ulcers and determination of sensitivity to antibacterial drugs are used. This way it is possible to determine which specific bacteria caused the inflammation. For deep tissue inflammation, a biopsy is also used.
In addition to examining the inflammatory elements directly, the patient is prescribed blood tests (clinical, blood glucose levels and other biochemical indicators), urinalysis, immunological and histological examination. This set of procedures allows you to accurately determine the pathogen, causes and type of skin disease.
Also, if necessary, the dermatologist prescribes consultations with other specialists - an endocrinologist, a therapist. A differential diagnosis is mandatory to exclude diseases with similar manifestations: tuberculosis, syphilis, candidiasis, microbial eczema, parasitic and fungal skin lesions.
Treatment of pyodermatitis in adults with immunotherapy
Immunotherapy is a method of treating pyodermatitis using drugs that stimulate the body's immune response to the effects of certain pathogenic microorganisms. Immunotherapy is prescribed for the chronic course of pustular disease with exacerbations of pyodermic lesions at least once every 3-4 months. Before prescribing a course of immunotherapy, the patient undergoes an immunogram, which allows one to evaluate the main characteristics of the patient’s immune system.
For the treatment of pyodermatitis in adults, the following immunological drugs can be used:
- Staphylococcal toxoid is a drug that promotes the formation of immunoglobulins (specific immune cells) that neutralize staphylococcus;
- Staphylococcal vaccine: this medicinal product has immunomodulatory and antimicrobial properties. The effect of the vaccine is to increase the number of immunoglobulins, which effectively resist infection, as well as stimulate the immune system;
- Staphylococcal bacteriophage is a specific virus that, penetrating into the cells of a staphylococcal infection, promotes their destruction;
- Streptococcal bacteriophage is a virus that destroys the cells of streptococcal bacteria;
- Leukinferon is a drug that contains interferon, which has immunostimulating properties. It enhances the immune system's response by affecting various immune cells;
- Streptococcal vaccine is a drug that activates the body's immune system to fight streptococcal infection.
Treatment of pyoderma
It is necessary to treat pyoderma under the supervision of a specialist; in no case should you use folk remedies or self-medicate! Such attempts can lead to serious deterioration of the patient's condition.
For superficial forms of diseases, the dermatologist prescribes surface antibacterial and antiseptic agents, aniline dyes (for example, brilliant green and other similar agents) that are suitable for a particular situation.
Complex cases include deep, overgrown, chronic and persistent pyoderma and relapses. If there is no effect from external therapy and there are complications (fever, inflammation of the lymph nodes), as well as inflammation on the face, the doctor prescribes oral medications: antibacterial, immunomodulatory. Also, if necessary, systemic retinoids and glucocorticosteroids are prescribed.
Low-intensity laser blood irradiation (LBI) is successfully used in the complex treatment of pyoderma. This procedure is especially relevant for stable and recurrent variants of the disease.
During the procedure, a light wave of a certain length and strength enters the bloodstream, knocks electrons out of blood cells and thus changes their structure. As a result, regeneration processes are launched and enhanced. Laser irradiation has several effects at once: strengthens the immune system, reduces the negative consequences of a previous illness, relieves swelling and inflammation, improves microcirculation and relieves pain.
The Altermed clinic has been successfully using an integrated approach to the treatment of pyoderma for 20 years - therapy, physiotherapy, immunocorrection. In addition to drug and immunocorrective therapy, the clinic’s doctors use narrow-band light phototherapy, physical therapy, and laser irradiation (ILBI). For each patient, an individual treatment plan is drawn up in accordance with the characteristics of the disease and the general condition of the body.
Material and methods
At the screening stage, 55 patients were observed. Before prescribing systemic therapy, all patients underwent bacterial culture for sensitivity to minocycline
. After the study, sensitivity was detected in 46 (83.6%) patients, who made up the observation group.
Subsequently, 46 patients aged from 18 to 67 years were under our observation - 24 (52.2%) men and 22 (47.8%) women. In 25 (54.3%) patients, the process arose for the first time (duration up to 2 months) and was of an acute inflammatory nature, in 21 (45.7%) it lasted more than 2 months (chronic inflammation). The following clinical forms of pyoderma were diagnosed: vulgar impetigo - 6 (13%) cases, boils - 10 (21.7%), periungual phlyctena - 9 (19.6%), pyoderma of large folds - 11 (23.9%), erysipelas - 10 (21.7%) (Fig. 1).
Rice. 1. Clinical forms of pyoderma in patients under observation.
Initial dose of Minolexin
was 200 mg (2 capsules of 100 mg or 4 capsules of 50 mg), then patients took 100 mg (1 capsule of 100 mg or 2 capsules of 50 mg) every 12 hours (2 times a day). The drug intake was independent of food intake. The duration of antibiotic therapy was 7 days, for erysipelas - 10 days. Depending on the severity of the process, patients used aniline dyes and antiseptic drugs as topical therapy.
Prevention of pyoderma
The first and most important rule for the prevention of pyoderma is timely antiseptic and antibacterial treatment of any wounds, cracks and microtraumas of the skin. Even habitual shaving causes microtraumas - pay special attention to the treatment of the skin and its daily care.
If you have diseases that increase the risk of developing pyoderma, treat them promptly in accordance with your doctor's recommendations.
If you already have a history of inflammatory skin diseases, do not forget about selective phototherapy and sanitation of focal infections. A detailed list of recommended procedures will be provided by a dermatologist.
Other articles by the author
- Pyoderma
- Herpes zoster
- Pityriasis rosea
- Shingles