Actinic keratosis is a pathological change in the skin caused by direct and prolonged exposure to solar radiation. This pathology develops over many years. Therefore, this disease is rare in young children. But in older people - quite often.
Interesting: In the keratosis classification system, the actinic form is identified as a separate disease, along with follicular, seborrheic, senile and hyperkeratosis.
Lesions may appear at a younger age in people who spend a lot of time outdoors and exposed to sunlight.
Interesting: An increased concentration of people with solar keratosis as a percentage of the total population is observed in areas with a large number of cloudless days a year.
If we talk about professional activities, then at risk are builders, beach lifeguards, road workers, guides - all those who spend a lot of time on the street and do not use protective cream.
Important: Experts note that actinic keratosis most often affects people of the “Scandinavian type” with fair skin, blue or green eyes and blond hair. Their bodies are deficient in protective pigment, which makes them susceptible to sunburn.
Causes of solar keratosis
As already mentioned, the cause of solar keratosis is sunlight, its frequent exposure to certain areas of the skin - the face, neck, nose and ears, hands and bald patches on the head, the area around the eyes. Foci of pathology can also appear on the back and chest if a person takes sunbathing or spends a lot of time in the sun without clothing.
The skin is damaged by ultraviolet radiation. With measured exposure to the open air, the skin quickly recovers. However, with excessive exposure, with weakened immunity, some areas of the skin cannot cope. That is, solar keratosis of the skin is not the consequences of a recent tan, but the result of many years of photo exposure.
Risk factors:
- Age over 40 years;
- Living in hot countries;
- Frequent tanning and sunburn;
- Light skin type, blond or red hair, blue or green eyes;
- Previous actinic keratosis or skin cancer;
- Weak immune system due to chemotherapy, leukemia, AIDS, or previous organ transplantation.
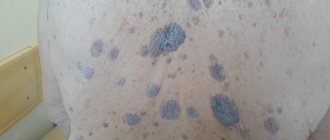
Rice. 3a. Actinic keratosis capitis
Rice. 3b. Actinic keratosis on the nose
Rice. 3c. Actinic keratosis on the face
Rice. 3g. Actinic keratosis on the forehead
Rice. 3d. Actinic keratosis at the corner of the eye
Solar keratosis symptoms
Actinic keratoses appear as red or pink patches on the skin that are flat or slightly raised. There are single and multiple manifestations. The size of single spots varies from a few millimeters to 3 centimeters in diameter. The spots themselves are dry and rough. Scales and crusts appear on the skin in the affected area.
Several elements can merge into one lesion, forming a large, rough area on the skin. Rarely, a conical neoplasm grows from the lesion. This pathology is called “cutaneous horn”.
There are no other symptoms. Actinic keratosis lesions do not itch or hurt. But spots can significantly spoil the appearance, as they are localized in open areas of the body. There is also a low risk of keratosis degenerating into a malignant form. Therefore, it is recommended to treat the pathology.
Etiology and pathogenesis of keratosis
One of the significant factors in the development of keratosis is constant exposure to ultraviolet radiation . A special role is played by ultraviolet light B (UVB, 290–320 nm) and A (UVA, 320–400 nm) - it induces p53-dependent apoptosis of epidermal keratinocytes. These apoptotic keratinocytes are often called “sunburn cells” (SBCs) and can be detected by histological examination of epidermis that has been overexposed to sunlight or tanning bed lamps.
In the development of keratosis, the UV-induced mutation of the tumor suppressor gene TP53, which is related to the above-mentioned p53 protein, is of great importance. Basal keratinocytes with mutant TP53 do not undergo apoptosis, which allows them to pass on genetic abnormalities to new cells. Similar changes are found in squamous cell carcinoma and other malignant tumors.
Actinic keratoses may be promoted by a general suppression of the body's immune response. The risk group includes patients who have undergone organ or tissue transplantation and are taking immunosuppressants.
Some medications can act as photosensitizers, increasing the skin's sensitivity to ultraviolet light and promoting the development of keratoses cutis.
Microscopy of keratotic lesions usually reveals dysplastic changes in the basal layer of the epidermis, accompanied by parakeratosis and solar elastosis of varying severity. An increase in the size and pleomorphism of nuclei, hyperchromatosis, an increase in mitotic activity or an atypical nature of mitoses, and cytoplasmic pallor are recorded.
Dysplastic epidermal growths may extend deep into the papillary dermis and in some cases are difficult to distinguish from superficial invasive squamous cell carcinoma of the skin. Dysplastic epidermal changes, as a rule, do not affect skin appendages (sebaceous and sweat glands, hair, nails) ( Fig. 1 ).
Rice. 1. Histological features of keratosis (www.medscape.com)
In the epidermis, moderate hyperkeratosis is observed with dysplasia of basal keratinocytes and the formation of small outgrowths extending into the papillary dermis. The presence of solar elastosis is noticeable. Dysplastic changes primarily affect the interfollicular epidermis.
Diagnostics
As a rule, diagnosis of solar keratosis does not cause difficulties, although outwardly the pathology looks like seborrheic keratoma. But an experienced dermatologist determines “sun damage” based on clinical signs. To confirm the diagnosis, instrumental research methods are used - dermatoscopy.
A dermatoscope is a digital magnifying glass that magnifies the skin pattern many times over. The device helps to identify benign formations and oncological tumors. Determine whether the patient has solar keratosis or Bowen's disease. In special cases, when basal cell carcinoma (malignant tumor) must be excluded, histology of tissue samples can be performed. But, as a rule, this is not necessary.
Keratoma removal Price
Keratoma, the removal of which by laser is relatively inexpensive, can be removed at different prices: the price range for laser keratoma removal is determined by the number of skin defects to be removed, their depth, complexity and other characteristics.
Our hair removal and cosmetology center “SkinLazerMed” specializes in a wide range of procedures that involve laser technology. We guarantee high-quality and painless keratoma removal on the same day of treatment.
How is the Laser Keratoma Removal procedure performed?
Removing a keratoma in this way is based on a laser beam affecting the affected area of the skin.
- Before starting the procedure, the dermatologist collects an anamnesis, finds out the characteristics of the patient’s health condition, possible contraindications to these manipulations, and tolerability of medications. These data allow you to determine the optimal power of the laser beam and the duration of its exposure, which allows you to perform the removal in one visit.
- A powerful cooling system is built into the equipment intended for exposure, this explains the comfort of laser keratoma removal. However, if the patient wishes, a subcutaneous injection of an anesthetic can be given to ensure that no discomfort occurs during the session.
- When it comes to a disease such as keratoma, laser removal is represented by stepwise “evaporation” of the affected tissue until the beam reaches a healthy layer of skin. During this procedure, bleeding occurs extremely rarely, but a small wound appears on the affected area. It is treated with antiseptic medications.
- The removed formation - keratoma, laser removal of which should be carried out only by a highly qualified specialist, should be monitored by a doctor for several more weeks.
The SkinLazerMed clinic will perform laser keratoma removal at an affordable price. The procedure is quick, effective and completely painless.
Actinic keratosis: treatment
Many experts argue that actinic keratosis may not be treated at all. After all, pathology in most cases does not pose a threat to health, and cases of regression are known. A therapeutic strategy such as observation is justified if a single lesion of small diameter does not affect the appearance and is not considered a cosmetic defect.
However, if additional symptoms appear - changes in shape, pain, redness of the skin around the lesion, you should consult a dermatologist.
Removal of actinic keratosis is the only way to treat this skin pathology. There are several methods to solve the problem. The doctor determines the optimal one, depending on individual characteristics - the number and location of lesions, diameter and thickness.
- Treatment with liquid nitrogen. The lesion is cauterized with the substance, and after the wound heals, the pathology disappears. But due to the impossibility of precise exposure to nitrogen, the skin around it can also be damaged. The wound takes a long time to heal. The advantage of cryodestruction is its affordable cost and relative ease of manipulation.
- In some cases, surgical removal of the lesion is performed. The disadvantage of excision with a scalpel is the high risk of scar formation at the site of exposure. And the wound after the operation takes a long time to heal.
- Laser treatment of actinic keratosis involves the removal of pathological tissue using a laser device, widely used in modern dermatology.
The laser method is considered the most effective and safe. There are reasons for this:
- Targeted impact.
- High speed of the procedure.
- Painless.
- There is no risk of bleeding or infection of the wound.
- Short rehabilitation period.
- Minimum list of contraindications.
You can learn more about the methods of treating solar keratosis used in dermatology and about the advantages of the laser method during a face-to-face consultation at the specialized medical Center for the diagnosis of moles “Lazersvit”. We offer highly qualified assistance in the diagnosis, treatment and prevention of various types of skin pathologies. We will be happy to help you.
Introduction
In recent years, the incidence of skin diseases associated with ultraviolet radiation has increased sharply.
These diseases primarily include actinic keratosis (AK), also known as solar keratosis, which is the most common precancerous skin growth [1, 2]. The first mentions of ACT date back to the end of the 19th century, but already to the beginning of the 20th century. started talking about the malignant potential of this disease [5]. Moderately expressed AK occurs frequently with a predominance of 15.4 and 34% of men and 5.9 and 18.2% of women at 40 and 70 years of age, respectively. The high incidence of AK is primarily associated with the cumulative effect of exposure to the sun or irradiation in a solarium, i.e. It is not at all necessary to get sunburn; it is enough to receive the usual dose of solar radiation to exposed skin for a number of years for the average person. Due to the predominant damage to the skin of the face, neck, and back of the hands, patients develop cosmetic, personal, psychological and social problems.
The main risk factors are old age, light skin tone, frequent sun exposure throughout life and long-term immunosuppression [6, 8, 9]. It is important to note that although most cases of AK do not develop into invasive squamous cell carcinoma of the skin, the majority of invasive squamous cell carcinomas develop at the site of AK [10].
AK diagnostics
Currently, many methods are used to diagnose AK, including histological examination, cytological examination of the skin, ultrasound of the skin, and dermoscopic examination. AK is usually diagnosed clinically and confirmed by cytology and dermoscopic or ultrasound examinations. When the clinical diagnosis is doubtful or in cases of clinical signs indicating malignant degeneration of AK, histological examination is necessary.
Microscopically, AK is characterized by proliferation of intraepidermal keratinocyte atypia (large pleomorphic and hyperchromic nuclei) with loss of polarity and mitotic parameters. These cells are similar to keratinocytes in invasive squamous cell skin cancer, which subsequently leads to the degeneration of a number of AK lesions [3]. The incidence of invasive squamous cell carcinoma in patients with AK, according to various sources, is 5–20% within 10–25 years, and the rate of transformation of AK into squamous cell carcinoma is 0.1–0.24% within 1 year. It was found that 8.4–100% of patients with invasive squamous cell carcinoma on open skin areas had a history of AK [3].
Clinical picture
Clinically, AK manifests itself in the form of single or multiple erythematous, slightly infiltrated spots of small sizes with round or oval outlines, covered with tightly fitting gray or yellowish-brown scales, after removal of which a papillary, sometimes eroded surface is revealed.
Treatment methods for AK
Taking into account the above facts, the issue of treatment of AK is relevant. In accordance with Russian, American and European clinical guidelines, today there are several methods of treating AK. The choice of treatment method is determined by the number of affected areas, their size, duration of the disease and localization of the lesion, and also depends on concomitant diseases, desired cosmetic results and the wishes of the patient. Treatment methods for AK include surgical excision, curettage and electrocoagulation, laser destruction, photodynamic therapy, application of ointment with 5-fluorouracil, cryodestruction. The importance of curing AK explains such a wide range of methods used. At the same time, each of the methods used has a number of disadvantages.
Surgical treatment is used extremely rarely and only in cases where the AK is a dense plaque with the possibility of deeper invasion. The choice of this technique is usually determined by the presence of signs indicating a high likelihood of developing squamous cell carcinoma. After excision of the affected area, a cosmetic suture is applied, however, the likelihood of cosmetic defects with this method is very high.
Curettage is a type of surgical intervention to remove a tumor using curettage. This method is considered very outdated and is rarely used for the treatment of AK due to its lack of effectiveness, as well as the frequent occurrence of cosmetic skin defects after its implementation, the duration of skin restoration and frequent infection of the area where it is performed due to insufficient patient compliance with the doctor’s recommendations for care the corresponding zone.
Electrocoagulation is the destruction or destruction of a formation by cauterization with high-frequency electric current. The effectiveness of this method for the treatment of AK has not been confirmed by clinical studies, and the likelihood of scarring is high.
Dermabrasion is used to treat multiple AKs. Diamond cutters or wire brushes are used with rotation speeds ranging from 800 to 33 thousand rpm; the inconvenience of the method is that the patient must stay in the hospital for at least a week.
Three types of drug treatment for AK are widely known: applications of ointment with 5-fluorouracil - the action of the drug is aimed at disrupting DNA synthesis and inhibiting the division of pathological cells; the use of imiquimod - the action of the drug is aimed at stimulating the synthesis of interferon: a substance that destroys cancer and precancerous cells. Treatment with this drug lasts about 4 months; gel with diclofenac and hyaluronic acid is prescribed for highly sensitive skin to other types of medications. The active component in this case is diclofenac, its action is aimed at preventing the appearance of squamous cell carcinomas.
These treatment methods do not take into account the proliferative capacity of cells, which determines their ability to invade, which leads to relapse of the disease. Cryodestruction is a method based on the local effect of low temperatures on the affected tissues, however, the lesion is not always limited to the affected cells and healthy tissues are often affected. The changes occurring in the cells are associated with the transformation that the water in the cell undergoes: when cooled, it turns into ice directly in the tissues, respectively, the tissue cells are compressed by the ice. As ice crystals form, they rotate around the center of crystallization and literally “cut” cellular and intracellular membranes. During freezing, blood circulation stops, the delivery of oxygen and nutrients stops, all biochemical reactions stop and the cells die. In addition, freezing causes a jump in osmotic pressure that the cells cannot tolerate. Exposure to cold leads to irreversible tissue destruction - necrosis. However, unlike laser therapy, this method does not make it possible to determine the required depth of tissue damage, as a result of which healthy tissues suffer, which increases the regeneration period of the skin.
Treatment with laser destruction (CO2 laser) of AK occurs by grinding the upper layers of the skin, is used only in the initial stages of the disease, has a number of contraindications associated with the presence of concomitant diseases (diabetes mellitus, autoimmune diseases, psoriasis, etc.), old age [11–24]. In addition, cosmetic problems that arise after the use of these treatment methods significantly aggravate socio-psychological and interpersonal relationships for most patients, often causing anxiety and a decrease in quality of life.
Photodynamic therapy solves the issue of adverse cosmetic consequences [25] and more than others meets the requirements of the doctor and the patient, however, the economic costs of providing medical organizations with laser units and photosensitizers limit its widespread use. In the last 20 years, special attention has been drawn to the possibility of using hyperthermia, in particular laser-induced thermotherapy (LITT), as an independent organ-preserving therapeutic technology for some solid human tumors. The LITT method is based on local heating of the tumor to 43–45°C using a laser whose wavelength ranges from 800 to 1064 nm.
As a result of the effect of laser radiation on tissue, selective heating of atypical cells occurs, associated with an altered structure of the vascular bed in the area of the neoplasm, which leads to the formation of microthrombosis in the affected area and, as a consequence, to hypoxia of atypical cells, which in turn triggers the processes of necrosis and apoptosis. It is known that LITT allows one to achieve a consistently high cytodestructive effect on actively proliferating cells with minimal damage to surrounding healthy tissues. There are reports in the literature about the effectiveness of LITT for basal cell carcinoma, Kaposi's sarcoma, and it is emphasized that the method, unlike surgical excision, is not invasive, is not toxic compared to chemotherapy, and, unlike radiation therapy, does not involve ionizing radiation and provides better cosmetic effect [26, 27]. It is important to note that there are no data on studies examining LITT for AK in the available literature.
The prevalence of the disease, the threat of transformation into a malignant process, the patient’s awareness of cosmetic unacceptability, the adverse effect on the psycho-emotional sphere and social adaptation determine the relevance of this problem and the need to develop new effective means and treatment regimens [5, 26, 28, 29].
Clinical case
Patient K. born in 1945, retired. She was admitted in January 2022 to the Department of Dermatovenereology and Dermato-Oncology of the State Budgetary Institution of Healthcare of the Moscow Region MONIKI named after. M.F. Vladimirsky with complaints of a spot on the skin of his right cheek. She considers herself sick since June 2016, when, for no apparent reason, she noted the appearance of a red spot measuring 0.3x0.2 cm on the skin of her right cheek, which gradually increased in size. During the spring-summer period, I did not use sunscreen during my life. On examination: on the skin of the right cheek there is a bright pink, rounded plaque with clear boundaries and a diameter of 0.7×0.6 cm, the surface of which is covered with scales and crust (Fig. 1). General condition is satisfactory.
Cytological examination results: changes in the dermis are represented by keratinocyte dysplasia and hyperkeratosis.
Ultrasound of AC formation revealed an increase in the thickness of the epidermis in the form of a strip of increased echogenicity and a hypoechoic zone, occupying a third of the dermis, corresponding to solar elastosis. Based on complaints, anamnesis, clinical picture of the pathological process, and examination data, a diagnosis of “actinic keratosis, erythematous form” was established.
The patient underwent LITT; a semiconductor laser device LAMI was used as a source of laser radiation (registration number 29/10020203/5212-03 [05/20/2003], code - OKP 944420, class - IIA, wavelength - 1064 nm, radiation power at the end of the fiber – 2.5 W).
A flexible quartz monofilament light guide with a diameter of 0.06 cm was used to supply light. To measure the laser radiation power at the light guide output, a DI-6A power meter was used. An assessment of the temperature field and the temperature achieved when exposed to laser radiation was carried out before the start of the study using the CEDIP IR camera.
Previously, intradermal infiltrative anesthesia of the tumor area was performed with 0.5 ml of a 2% lidocaine solution. After 5 minutes, the end end of the light guide was brought to the surface of the tumor by 0.2 cm without direct contact with the surface of the skin. The exposure lasted for 10 minutes. Directly during and immediately after the LITT procedure, signs of hyperemia and slight swelling of the surrounding tissues were noted in the area of the lesion. The treatment was well tolerated. No changes in general condition were observed. After 3 days, slight peeling of the skin was visualized at the site of lesion destruction; there were no subjective sensations.
The effectiveness of LITT was determined at the end of the therapy session, 24 hours later, on the 3rd day after treatment, as well as after 3, 6 and 12 months.
The treatment effectiveness was assessed according to the following criteria:
- regression of the lesion - the absence of a visible and palpable lesion with confirmation of the absence of atypical cells by cytological or histological studies;
- partial regression - a decrease in size by more than 50% or a visible absence of the lesion, but when atypical cells are detected in the cytological or biopsy material;
- no effect – reduction in the size of the lesion by less than 50%, the condition is unchanged and an increase in the size of the lesion.
When assessing the cosmetic effect, the presence or absence of a scar, atrophy, skin thickening, pigmentation or hypopigmentation, and hyperemia was taken into account.
3 months after treatment, an area of congestive hyperemia of a violet-pink color formed at the site of a pre-existing AC lesion; a pseudo-mesh with foci of hyperpigmentation, branching structures forming a rounded lesion with clear boundaries and “ragged” edges was visualized dermoscopically in the field of view, with ultrasound of the area of the previously existing formations in the epidermal zone there was no band of increased echogenicity and a hypoechoic zone in the dermis.
After 6 months, an area of pink hyperemia clinically remained in the area of the treated AC lesion. After 12 months, slight hypopigmentation remained clinically in the area of the pre-existing AK lesion (Fig. 2). Cytologically, there was no keratinocyte dysplasia or hyperkeratosis.
The cosmetic result was assessed as good (an area of slight hypopigmentation remained).
In order to prevent the appearance of new lesions of AK, the patient was recommended to avoid sun exposure and use sunscreens with the maximum protection factor when going out in the sun.
Conclusion
The prevalence of the disease, the threat of transformation into a malignant process, the patient’s awareness of cosmetic unacceptability, the adverse effect on the psycho-emotional sphere and social adaptation determine the relevance of this problem and the need to develop new effective means and treatment regimens.
We believe that the LITT method is interesting for further study in relation to the treatment of AK.