Any deviations from the norm in newborns instill panic and fear in new parents. Hemangioma, which is a tumor-like formation, is no exception. It is formed by endothelial cells, or small capillary vessels. Most often, hemangiomas occur on the head, chest and back, increasing in size in the first year of a child’s life. The tumor usually goes away as the child grows older, but in some cases it can harm health by interfering with normal breathing or negatively affecting visual function.
Hemangioma in a newborn
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Treatment methods
- Medicinal methods
- Surgical methods
- Hardware methods
Hemangioma (capillary hemangioma, capillary hemangioma) is a benign tumor that develops from hyperplastic vascular endothelium. It is often absent at birth, but appears in childhood and is characterized by progressive growth.
In our company you can purchase the following equipment for removing hemangiomas:
- M22 (Lumenis)
- AcuPulse (Lumenis)
- Fraxel (Solta Medical)
- UltraPulse (Lumenis)
A feature of hemangiomas is the possibility of spontaneous involution, therefore the treatment tactics for these neoplasms are selected individually for each patient, based on the current state of the tumor and its dynamics. Spontaneous regression distinguishes hemangiomas from other vascular malformations, such as port-wine stains.
According to statistics, capillary hemangiomas occur in 1–2% of newborns, with about 50% of neoplasms forming on the head (often in the eye area) and neck. 30% of patients say that their parents or doctors recorded signs of hemangioma immediately after birth, but the majority note the onset of manifestation of this neoplasm at the age of 6 months. The ratio of men to women in the incidence of hemangioma is 1:3.
Education mechanism
Medicine has not found any exact reasons why this type of tumor forms on a baby’s body. There are more hypotheses than facts, despite the fact that many years of research into infant hemangiomas have been conducted.
Doctors are convinced of only one thing - the reasons are not genetic, therefore heredity in the formation mechanism is excluded by almost all specialists.
Development of hemangioma
However, there are aspects whose participation in the formation of hemangiomas is assumed with a high degree of probability.
- ARVI suffered by a pregnant woman in the early stages, between the third and sixth week. It is during this time period that the formation of the cardiovascular system of the embryo occurs.
- Rhesus conflict, when positive red blood cells from the fetus enter the maternal bloodstream.
- Pregnant women taking medications not authorized by a doctor, smoking during pregnancy, drinking alcohol.
- The presence of hormonal imbalances and disorders in both the fetus and its mother.
- Low level of ecology where the pregnant woman lives.
- Heredity aggravated by any vascular disease.
- Multiple pregnancy (starting with twins).
- The age of the woman giving birth is over 38 years.
- Birth of a child prematurely.
- Convulsive seizures in a pregnant woman.
In multiple pregnancies, there is a risk of developing hemangiomas in children
Bad habits increase the risk of developing fetal pathologies
If we briefly characterize the hypothesis of the mechanism of formation, it will sound like this. At the stage of bearing a child, when its cardiovascular system is formed, endothelial cells, under the influence of some (not precisely established) factors, are sent to the “wrong address”. Instead of forming the inner surface of the blood vessels, they form a tumor.
Bandages for pregnant women
If you want to find out in more detail what symptoms spinal hemangioma has, and also consider alternative treatment methods, you can read an article about this on our portal.
Etiology and pathogenesis of capillary hemangiomas
Today, it is believed that capillary hemangioma is a hamartomatous proliferation (i.e., a nodular benign tumor-like formation representing a tissue developmental abnormality) of vascular endothelial cells. To date, no specific gene mutations or obvious hereditary characteristics have been found that would be 100% responsible for the appearance of hemangiomas.
In its development, hemangioma goes through 2 phases - proliferative and involutive. The proliferative phase usually begins 8–18 months after tumor manifestation and is characterized by progressive growth of the tumor. Histologically, it is characterized by an increase in the number of endothelial and mast cells, the latter stimulating further vascular growth.
The proliferative phase gives way to the involutive phase , which is characterized by gradual regression of the hemangioma. It exhibits a reduction in angiogenesis, apoptosis of endothelial cells, a decrease in the activity of mast cells and dilation of vascular channels. About 50% of all neoplasms undergo involution before the age of 5 years, and about 75% - before the age of 7 years.
Clinical manifestations
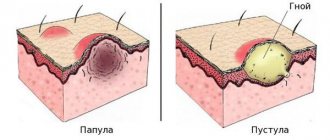
A simple hemangioma is a red, bumpy neoplasm that rises above the surface of the surrounding healthy skin ( Fig. 1 ). Cavernous hemangioma is located in the subcutaneous fatty tissue and looks like a bluish tumor ( Fig. 2 ). Combined hemangioma is located both on the surface and inside the skin. There are also mixed hemangiomas , which are combined with lipomas, fibromas, keratomas and other neoplasms.
An important differential feature of hemangiomas is blanching when pressed - this distinguishes them from port-wine stains.
Rice. 1. Simple capillary hemangioma
https://www.danderm-pdv.is.kkh.dk/atlas/7-65.html
Rice. 2. Cavernous hemangioma
https://www.danderm-pdv.is.kkh.dk/atlas/7-69-2.html
Depending on the location, hemangioma can cause various complications. Thus, a periobrital tumor in 43–60% of cases provokes amblyopia - “switching off” the affected eye from the visual process. Located in the larynx, the tumor can cause stridor and airway obstruction. In general, despite the benign nature of hemangiomas, about 10% of them are destructive in nature, causing serious aesthetic defects.
Symptoms
Spinal hemangioma does not manifest itself in any way until the integrity of the vertebral body is compromised and the above-described disorders occur. Only in very rare cases is radicular syndrome observed, i.e., pinching of the nerves passing through the affected vertebra and the occurrence of:
- sharp, shooting pains along its course, caused by various movements, coughing, laughter;
- sensations of numbness, crawling;
- limited movement.
If the hemangioma is located in the cervical vertebra, cerebral circulation may be impaired, which will lead to headaches, dizziness, hearing, vision and sleep disturbances. When it is localized in the thoracic vertebra, disturbances in the functioning of the pelvic organs, heart, and digestive organs may be observed, and when a tumor forms in the lumbar vertebrae, there are frequent cases of pain radiating from the lower back to the groin and hips.
This is only possible when the hemangioma reaches a large size and leads to a compression fracture of the spine without the formation of individual bone fragments, which occurs only in 0.1% of patients with vertebral hemangioma. In such situations, the vertebra seems to be evenly flattened. As a result of a decrease in its height, the size of the natural openings through which the nerves pass also decreases, which leads to their compression and the development of radicular syndrome.
In the vast majority of cases, radicular syndrome occurs due to intervertebral hernia.
The patient must clearly understand that hemangioma, although it is a tumor, has nothing to do with oncology and is not capable of degenerating into a malignant neoplasm and giving metastases. This is very important to reduce stress levels and avoid the development of anxiety, since negative experiences weaken the body and false back pain may occur, which significantly reduces the quality of life.
Treatment methods for hemangiomas
Primary therapy for capillary hemangiomas is simple dynamic observation . Since most tumors (up to 75%) regress with age, there is usually no need for their treatment. However, hemangiomas can cause complications that require therapy:
- Systemic complications - congestive heart failure, thrombocytopenia, hemolytic anemia, nasopharyngeal obstruction.
- Ophthalmological complications - disturbance of the visual axis, compression of the optic nerve, severe proptosis (protrusion) of the eyeball, anisometropia (difference in eye refraction).
- Dermatological complications - maceration and erosion of the epidermis, infection of the neoplasm, severe cosmetic defect.
Medicinal methods
Depending on whether the patient has a particular complication, treatment tactics will be different - for example, topical corticosteroids may be prescribed. At the same time, the clinical response to even the most powerful drugs develops quite slowly—over several weeks. Therefore, this method is not suitable for vision-threatening conditions.
Injectable corticosteroids provide a faster effect: blanching of hemangiomas is observed already on days 2–3, and involution becomes noticeable after 2–4 weeks. The success rate of this therapy is about 75%.
Systemic corticosteroids are used for amblyogenic life-threatening lesions. A marked response is usually observed in 30% of patients, a moderate response in 40%, and no response in 30%.
Alpha-2a interferon is prescribed when hemangioma is resistant to corticosteroid therapy. Despite its good effectiveness, its use is associated with undesirable side effects: fever, arthralgia, retinal angiopathy.
Propranolol can be used to treat hemangiomas , although the evidence base is relatively weak and mainly consists of anecdotal cases. However, some studies indicate that propranolol may prevent loss of visual acuity in the case of periocular hemangioma.
For some superficial (and in some cases deeply located) neoplasms of a limited area, timolol .
Hardware methods for treating hemangiomas
CO2 laser was previously used to remove hemangiomas , which has a good hemostatic effect. The disadvantage of the CO2 laser is long-term rehabilitation due to damage to the integrity of the skin, as well as the formation of a scar at the site of the removed hemangioma. Pulsed dye laser ( PDL) is effective only for superficial tumors. Its effect develops quite slowly, which does not allow the use of the PDL laser for complications. Currently, intensive pulsed light - IPL and long-pulse Nd:YAG laser 1064 nm, as well as their combination, are used to treat hemangiomas for aesthetic purposes. These techniques are non-ablative and are based on selective heating of pathological vessels due to the absorption of light energy by hemoglobin.
Indications for removal
In the absence of direct medical indications, a wait-and-see approach can be applied to congenital pathologies, which often pays off. It is of little use to infant tumors, since during the period of intensive growth of the child they can significantly increase in size. In this case, removal of the vascular hemangioma is indicated.
Indications
- Ulceration
- Life-threatening location, e.g. respiratory tract, liver
- Tumor infection
- Growth in depth, which is accompanied by compression of healthy vessels and tissues
- Mechanical damage, etc.
Contraindications to the procedure
- Individual intolerance to laser radiation
- Oncology
- Exacerbation of chronic, infectious, seasonal diseases
- Immunodeficiency conditions
- Systemic blood diseases
- Diabetes mellitus, etc.
You can get acquainted with the full list of contraindications during a consultation with a doctor at our medical center in Moscow. Having studied the complexity of your problem, the specialist will answer all your questions, including whether it is possible to remove hemangioma with a laser in children of a certain age. Reception is by appointment only.