- Answers
Kostevich Galina Vladimirovna - Category:
Gynecologist-oncologist of the highest category - Experience: more than 25 years
The vagina of a woman or girl is not protected from the appearance of benign tumors. This usually occurs between the ages of 20 and 50. In the process of the emergence and development of neoplasms, cells of tissues such as adipose, connective and epithelial, as well as blood vessels, are involved. Tumors can be in the form of a dense single node with a wide base or a long stalk. Sometimes a benign neoplasm is a collection of multiple nodules. They are found under the mucous membrane of the vaginal walls. A specific feature of neoplasms of this type is their inability to disrupt the structure of the tissue. They just squeeze it. No metastases or relapses are detected. Tumors grow slowly.
Why are polyps dangerous?
The content of the article
Any polyps, no matter where they are located, should be treated. Even if the tumors are benign, the condition is diagnosed as precancerous. For women planning to have children, the pathology is especially dangerous, because it leads to infertility.
Let's consider 2 types of polyps:
- Adenomatous polyp.
A type of adenoma that manifests itself in the growth of endometrial tissue - the mucous membrane covering the inner surface of the uterus (during menstruation, the functional layers of the endometrium come out with secretions). Adenoma is a benign tumor and appears only in organs with glandular epithelium, but over time it can degenerate into oncology - cancer. The risk increases when the condition is neglected. Adenomatous polyp also appears on other organs, but its occurrence in the uterus is most life-threatening. - Glandular polyp.
Already from the name it is clear that this type of polyp is formed from glands and endometrial tissue. Such polyps are small and the safest among similar neoplasms. The diameter of a glandular polyp does not exceed 1.5 cm. Glandular polyps are almost always benign, although there are cases where endometrial cancer developed from just such a focus. It happens that the lumen of the glands forms a cyst, then a glandular cystic polyp is diagnosed. Glandular cystic polyp is not a separate subtype. Such polyps form in the form of a node and are located in the stroma of the mucous membrane, which is located in the places where the fallopian tubes drain.
Diagnostics
At the first appointment, the doctor is unlikely to be able to make a diagnosis, since it is impossible to determine the location of the polyp in the internal cavity of the uterus without a thorough examination. There are objective and subjective reasons that may raise suspicions of uterine polyposis.
Subjective signs:
- pain in the lower abdomen;
- general malaise.
Objective signs:
- results of general and biochemical blood tests;
- analysis of vaginal smears;
- gynecological ultrasound results;
- hysteroscopy.
If the diagnosis is confirmed by the gynecologist, the doctor gives a referral for a biopsy. Further treatment will depend entirely on the results of histological examination. In most cases, the treatment method for adenomatous and glandular polyps is surgery.
Therapy for pregnant women
Genital warts in the vagina can appear during pregnancy due to a weakening of the body's natural defenses. In this case, it is necessary to contact a gynecologist as soon as possible so that the specialist can conduct a comprehensive examination and identify possible concomitant diseases, such as thrush. Surgical removal of genital warts is not performed during pregnancy, since any surgical interventions are contraindicated for the expectant mother.
Specialists limit themselves to local therapy, which eliminates itching, inflammation, and prevents the occurrence of infectious complications and frequent relapses of the disease. Topical antiviral drugs should be used only after the permission of the attending physician.
But sometimes local treatment of vaginal condylomas does not bring the expected result. This is all due to a natural decrease in immunity, which allows you to maintain the viability of the fetus and avoid miscarriage. Also, an exacerbation of human papillomavirus infection is caused by hormonal changes in a woman’s body.
If local medications do not help get rid of vaginal condylomas, it is recommended to wait a while, using daily antiseptics and other safe means that will inhibit the growth of the virus. After childbirth, in most women, vaginal warts completely disappear, which indicates a connection between human papillomavirus infection and natural changes in the body of the expectant mother.
Uterine polyps
The uterus is a hollow organ of the female reproductive system, the inner surface of which is lined with a mucous membrane - the endometrium. The endometrium has specific physiological and functional properties. Sometimes there is a pathological growth of the glandular structures of the endometrium - a polyp of the uterine body, which most often is not classified as an oncological condition.
Polyps of the uterine cavity can have different shapes, sizes and locations, which directly determines the impact of such a neoplasm on a woman’s reproductive and sexual health. Since any polypous structures are prone to further growth, doctors recommend getting rid of polyps of the uterine body immediately after detection.
Causes of uterine polyps
Until recently, gynecologists considered polyps to be a consequence of previous pregnancy and childbirth, but in recent years, polypous neoplasms are increasingly being diagnosed in adolescents and young nulliparous girls, and are also found in women of menopausal age.
Based on research results, it was found that the main reason provoking pathological growth of the endometrium is hormonal disorders. This explains the frequent manifestation of the disease during pregnancy, lactation and puberty. In addition, polyps can result from erosion, injury to the endometrium during surgery, as well as complications from inflammatory processes in the mucous membrane.
Symptoms of polyps in the uterus
A single polyp of the uterine cavity, like multiple polyposis, may not appear for a long time, being completely asymptomatic. Often the patient learns about the development of such a structure only when the polyp is injured or torn off. Paying close attention to your own health will help you identify polyps by the following symptoms:
- Vaginal bleeding or light spotting a few days after menstruation;
- A feeling of discomfort or even mild pain during sexual intercourse;
- Long-lasting nagging pain in the lower abdomen;
- Irregularities in the menstrual cycle.
If you notice any sign of the above symptoms, you should immediately seek professional medical help.
Diagnosis and treatment of uterine body polyps
There are several ways to diagnose a polyp of the uterine body:
- Ultrasound confirmed by colposcopy;
- Hysteroscopy – visual examination of the uterine cavity using special optical equipment;
- X-ray examination of the uterus - metrography.
After establishing the presence of a polypous structure, the specialist determines the preferred method of removing the tumor. The most commonly used technique is polypectomy, which involves unscrewing the body of the polyp and cauterizing the base using an electric current. There is also a less traumatic method - removal of polyps using radio wave surgery. Our clinic uses the new Fotek radio knife.
For multiple polyps, curettage of the uterine cavity is practiced. Polyps removed during the intervention and the surrounding tissue are sent for histological examination (cancer testing). If the analysis reveals the presence of atypical (degenerated) cells, the doctor suggests a possible oncological process.
If you notice signs of pathology, contact the Diana Medical Center. Here, diagnosis and treatment of uterine body polyps can be carried out using the latest expert-class equipment under the professional supervision of highly qualified specialists.
Cervical polyp
A cervical polyp is a benign neoplasm that is formed through pathological growth of the epithelium (covering tissue) lining the cervical canal. Such structures can have different shapes and sizes, however, regardless of these characteristics, if such a growth is detected, it is necessary to remove it, because polyps negatively affect the reproductive and sexual function of a woman.
Cervical polyps are also dangerous for other reasons - there is a high probability of injury to them, and malignant degeneration of the tumor is also possible. A woman of any age can encounter a similar problem, but the greatest risk is observed during periods of serious hormonal changes - puberty, pregnancy, menopause, etc.
Reasons for the formation of cervical polyps
Often, cervical polyps form without any apparent reason and do not make themselves felt for a long time, developing asymptomatically. However, several key factors have been identified that increase the risk of developing polyps in the cervical canal:
- Hormonal imbalance.
This reason can be either age-related or physiological in nature (menopause, pregnancy), or develop against the background of gynecological pathologies such as uterine fibroids, ovarian dysfunction, endometriosis. - Psycho-emotional stress.
Long-term exposure to stress factors, overwork, nervous instability - all this can provoke the proliferation of epithelial (integumentary) tissues of the cervical canal against the background of a decrease in natural immune defense. - Mechanical injury.
Gynecological manipulations such as diagnostic curettage or hysteroscopy may be accompanied by damage to the mucous membrane of the cervix, which subsequently leads to the formation of polypous structures. - Infectious and inflammatory processes.
Any inflammation of the cervix, such as endocervicitis or the consequences of an infectious process, is combined with the risk of developing a polyp.
Symptoms of cervical polyps
The first signs of polyposis often develop when the neoplasm has already reached a significant size. At this time, women note constant nagging pain in the lower abdomen, discomfort and pain during intimate life and sexual arousal, and uncharacteristic vaginal discharge (leucorrhoea, bloody, serous). These symptoms manifest themselves especially clearly during menopause, when any bleeding is considered a reason to seek medical help.
Quite often the formation of polyps is accompanied by infertility. If pregnancy occurs despite polyposis, experts recommend postponing treatment until the postpartum period, and only in rare cases is surgical removal of such tumors prescribed in the early stages of pregnancy.
Diagnosis and treatment
The presence of a cervical canal polyp can be detected during a classic gynecological examination. Confirmation of the diagnosis requires colposcopy and cervicoscopy or a gynecological ultrasound procedure. The method of removal is determined by the specialist individually, based on the age and health of the patient, as well as the size and location of the tumor.
Most often, polyps are removed using palipectomy or the radio wave cold method - this is a low-traumatic modern procedure. If the gynecologist considers it necessary, curettage of the epithelium is performed.
Vaginal polyp
Vaginal polyps are benign neoplasms that grow on the mucous membranes and epithelial (integumentary) tissues. One of the places where polypous structures are localized is the vagina. The formations in this case most often represent multiple small tubercles with a wide base.
There are several reasons that provoke the development of pathological proliferation of vaginal tissue, however, regardless of the factor that caused the process, polyps in the vagina must be removed.
Preventive actions
After getting rid of HPV, lifelong immunity does not appear. The growths in the vagina may reappear after treatment. This happens due to the activation of a virus already in the body or due to infected sexual partners.
Preventive measures consist of:
- strengthening the immune system;
- healthy lifestyle;
- prohibition on uncontrolled sexual relations;
- using condoms during sexual acts;
- timely treatment of diseases;
- periodic examinations by a doctor.
These simple tips will reduce the risk of condylomas in the vagina and curb the activity of HPV, which is already present in a woman’s body. And if symptoms begin to appear again, you need to urgently consult a doctor.
Causes of formation of vaginal polyps
There are several reasons that provoke the growth of polyps:
- Human papillomavirus.
Papillomavirus has more than a hundred varieties, each of which forms a priority location for localization. This type of papilloma, such as genital warts, quite often affects the mucous tissues of the genital organs, including the vagina. They usually visually resemble lobed cauliflower, being reddish-pink in color. Polyps caused by the human papillomavirus usually show multiple growths and are localized close to the vaginal opening. - Mechanical damage to the mucous membrane.
Injuries to the vagina during medical procedures and childbirth, accompanied by ruptures of the mucous membrane, inevitably lead to the formation of a scar. Over time, individual polyps may appear in an area of rough connective tissue. - Chlamydia and other sexually transmitted infections.
The infectious-inflammatory process is one of the leading factors stimulating the formation of vaginal polyps. - Hormonal disorders.
Hormonal changes, as well as diseases accompanied by endocrine imbalance, often contribute to the formation of polyps. Sometimes the process of polyp growth itself occurs in the cervical canal, and after that the body of the neoplasm falls into the vaginal lumen, where it is diagnosed.
Symptoms of vaginal polyps
Vaginal polyps may not show any specific symptoms for a long time. However, some women report itching and burning of the affected area, which most often occurs after sexual intercourse.
During intimate intimacy, due to trauma to neoplasms, bleeding or scanty sanguineous discharge may develop. In some cases, pain and discomfort in the lower abdomen are noted, but this phenomenon is relatively rare.
Treatment of vaginal polyps
The presence of pathological growth of the vaginal mucosa is usually detected during a standard vaginal examination, which can be supplemented by colposcopy for final confirmation of the diagnosis.
Unlike polyposis of the body or cervix, vaginal growths can be eliminated using techniques such as laser and radio wave correction, cryodestruction, electrocoagulation and chemical removal. The use of the latter technique is limited during pregnancy. Having determined the cause of the development of polyposis, the specialist will also prescribe treatment aimed at eliminating the factor that caused the disease.
Benign tumors of the vagina
Fibroma, myoma, vaginal lipoma
True benign tumors of the vagina include fibroids, myomas, fibromyomas, and lipomas.
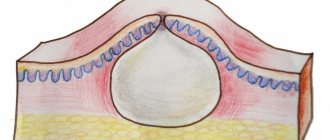
The growth of benign vaginal tumors is based on the proliferation of connective (fibroma), smooth muscle (fibroids), and less commonly adipose (lipoma) tissue. True tumors are localized under the mucous membrane of the vaginal wall; may look like a single node with a wide base or a long leg; less often they are in the nature of multiple nodules. Clinically, vaginal tumors can manifest themselves as nagging or contact pain, foreign body sensation, discomfort during sexual intercourse, and disturbances in defecation and urination. Torsion of the leg or hemorrhage in the vaginal tumor tissue may be accompanied by necrotization, inflammation or suppuration. In rare cases, malignancy of benign vaginal tumors is observed.
True vaginal tumors are detected during a gynecological examination. During bimanual examination, a tumor associated with the vaginal wall is palpated, having clear boundaries, dense consistency, and limited mobility. When examined in the speculum, a node is found located in the area of the anterior wall, on a broad base or pedicle under the unchanged vaginal mucosa. The size of true vaginal tumors can reach a chicken egg. During transvaginal ultrasound, a solid structure of vaginal tumors is visualized, with average or reduced echogenicity, similar to uterine fibroids.
For asymptomatic vaginal tumors, they can be monitored dynamically. If there is a tendency to growth or clinical symptoms, vaginal tumors are removed surgically: they are peeled off from the submucosal layer within the bed or the stalk is cut off. The operation is often performed through a transvaginal approach; Deeply located vaginal tumors can be removed using abdominal wall transsection. The morphological form of the vaginal tumor is determined during histological examination of the specimen.
Papillomas (condylomas) of the vagina
Papillomas (condylomas) are tumors of the integumentary epithelium that look like papillary growths on the vaginal mucosa. Papillomas are a manifestation of a common human papillomavirus infection. They have exophytic growth, have a thin stalk or a wide base. Papillomas can manifest as itching, burning in the vagina, contact bleeding due to trauma, and unusual discharge. Papillomatous tumors of the vagina in some cases undergo decay or malignancy.
Diagnosis of papillomas includes cytological examination of a smear, colposcopy, biopsy of a vaginal tumor with histological examination, PCR determination of HPV with typing of non-oncogenic and oncogenic strains.
Removal of vaginal papillomas is strictly necessary and can be done with medication, liquid nitrogen, laser, electrocoagulation, plasma coagulation, surgical scalpel, or radio wave method. After removal of papillomas, immunomodulatory therapy is prescribed.
Vaginal hemangioma
Hemangiomas are vascular tumors of the vagina with a soft consistency. Based on their structure, capillary and cavernous hemangiomas are distinguished. Having arisen on the vaginal mucosa, hemangiomas can spread to the cervical canal and into the uterine cavity. In some cases, ulceration and necrosis of vascular tumors of the vagina are noted.
Vaginal hemangiomas often manifest themselves as contact bleeding due to trauma. When a vascular tumor of the vagina spreads to the internal genitalia, a clinic of hyperpolymenorrhea may occur.
During a gynecological examination, a vaginal hemangioma appears as a red, purple or bluish spot rising above the mucosa. Local swelling of the mucous membrane, loosening of the integumentary epithelium, and engorgement of folds are noted. During colposcopy, attention is drawn to the presence of an extensive network of anastomosing, and in some areas, varicose vessels.
Non-progressive, non-ulcerating, vascular tumors of the vagina that do not disrupt the ovarian-menstrual cycle can be left under observation. With a progressive clinical picture, vaginal hemangiomas can be removed surgically, using cryotherapy, electrocoagulation, or sclerotherapy.
Vulvar polyp
The vulva is the collection of external genitalia of a woman. Polyps often inhabit the areas of the labia, clitoris, and vestibule of the vagina.
Pathological growth of the mucous membranes is accompanied by the appearance of a growth or tubercle, which can increase in size or form lobular structures that look like cauliflower. Due to the open localization of tumors, they, unlike polyps of the uterine body or cervical canal, are much easier to diagnose and, as a rule, are removed at an early stage, which avoids the degeneration of the tumor into a malignant form.
Causes of vulvar polyps
Polyps are often called not classic polyps, but genital warts, the primary reason for the formation of which is the penetration of the human papillomavirus into the patient’s blood. Against the background of a reduced immune response and hormonal imbalance, the papillomavirus causes pathological division of epithelial cells, which ultimately leads to the growth of condylomas. At the initial stage, such structures may take the form of multiple tubercles, which, as they grow, merge into one voluminous tumor-like papilloma.
The main factor in the formation of vulvar polyps is mechanical trauma to the external female genitalia. The healing of the wound in this case is accompanied by the formation of a scar, the basis of which is rough connective tissue. It is this area that becomes the localization zone for single polyps.
Also, vulvar polyposis can occur against the background of hormonal changes, such as pregnancy, puberty or menopause, and inflammatory and infectious processes, usually sexually transmitted infections.
Diagnosis and treatment of vulvar polyps
Diagnosing vulvar polyps is not difficult. A gynecologist can make a diagnosis after a simple physical examination, which is often combined with a gynecological examination, in order to exclude the possibility of proliferation of vaginal and cervical polyps.
Removal of vulvar polyps can be done in the following ways:
- Laser technique -
the pathological growth is destroyed under the action of a directed laser beam. The technique is considered the least traumatic and, accordingly, the safest among all currently known methods of excision of epidermal tumors. - Radioknife
- radio wave therapy is preferable for any gynecologist. It has many advantages, including over laser removal. In particular, a radioknife can be used to take polyp tissue for analysis, while a laser evaporates the entire tumor. - Cryodestruction is
the freezing of pathological tissue areas by exposure to extra-low temperatures through applications of liquid nitrogen. - Electrocoagulation -
the technique involves the use of electric current as an aggressive destructive agent. - Surgical excision is
used relatively rarely due to the high level of trauma and the long period of tissue healing.
Treatment methods for condylomas
Most often, patients come to us with genital perianal condylomas, the removal of which can be carried out in various ways:
- radio wave therapy (removal of condylomas with a radio knife);
- cryodestruction (cauterization of condylomas with low-temperature liquid nitrogen);
- laser coagulation (evaporation of pathological neoplasms with a laser);
- electrocoagulation (use of high-frequency current).
To prevent recurrence of condylomatosis, antiviral therapy is prescribed. Patients are also advised to periodically visit specialists and get tested. Women who have had condylomas removed should have smears twice a year and undergo histological diagnosis.