Hyperkeratosis of the foot
— Plantar hyperkeratosis and thickening of the epidermis. Hyperkeratosis of the feet is characterized by rough and dry skin, cracking, painful and bleeding. The diagnosis of hyperkeratosis is made on the basis of an external examination of the foot performed by a dermatologist, podiatrist or podiatrist; the result of a skin biopsy followed by histological examination of the substance. Treatment of hyperkeratosis of the feet is complex: foot baths, foot covers, hardware therapeutic pedicure and the use of special cosmetics are effective for this.
general information
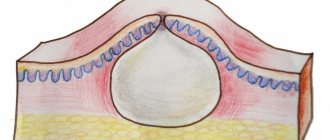
Hyperkeratosis of the foot (hard stratum corneum, abbreviated as adipose tissue) is a pathological growth of the stratum corneum of the epidermis, which reaches a thickness of more than one centimeter. Complications of hyperkeratosis may include minor patchy bleeding (bleeding), soft (between toes, nails) and hard (root) plaque, and ulcers caused by increased pressure in the foot. Bleeding and scabs are generally not harmful to health, but are a drawback to beauty and cause discomfort when walking.
They must be removed using special procedures. Foot ulcers are common in people with diabetes. In addition to cosmetic methods, they also have to treat serious diseases.
Cracking of the feet often occurs against the background of hardening of the stratum corneum, causing great discomfort. However, their development is not always directly related to hyperkeratosis; they can also be the result of improper care of the skin of the feet.
Hyperkeratosis of the foot
Causes of foot hyperkeratosis
In the case of hyperkeratosis, two groups of factors are distinguished:
External cause (external)
In this case, the cause of hyperkeratosis is increased stress and lengthening of certain areas of the foot. Under stress, skin growth cells begin to multiply rapidly. Under normal conditions, the upper cells of the epidermis gradually fall off, giving way to newly formed ones. Excessive cell division causes the top layer to fall off too late, thickening the stratum corneum. Hyperkeratosis.
One of the most common external causes of hyperkeratosis is unsuitable shoes. Wearing narrow and tight shoes not only puts too much pressure on the feet, but also treacherous and worn-out shoes or shoes that are oversized. Wear shoes that are too loose, your feet are not secured, and they can move while you walk, which can cause pressure and friction on your feet and cause illness.
Another cause of excessive foot pressure is body composition: weight gain and height. Besides,
Various foot deformities, including congenital (flat feet or femoral feet) and life-acquired (as a result of injury or surgery), can also cause hyperkeratosis. In this case, the load on certain areas of the foot is several times higher than the physiological norm, and these areas are subject to excessive pressure.
Internal reason (internal)
These are mainly endocrine and skin diseases. You have diabetes, a disorder of carbohydrate metabolism in the body. This, in turn, can lead to changes in pain in the lower extremities and touches, impaired circulation and tissue nutrition, dry skin, ulcerative lesions and other risk factors for the development of hyperkeratosis.
Hyperkeratosis can also be caused by a variety of skin conditions, including psoriasis, palmoplantar keratosis, ichthyosis, and congenital disorders of keratin synthesis.
The combination of several factors (endogenous and exogenous) increases the risk of developing and developing hyperkeratosis. For example, in patients with diabetes, wearing tight shoes may have the most adverse effects on the development of iron ovaries.
Treatment of foot hyperkeratosis
Family therapy
Excessive keratosis of the foot without salon surgery requires careful home care.
The enemies of hyperkeratosis are regular hygiene procedures and emollients. As a “family doctor” it is recommended to use preparations of lavender, mountain pine, rosemary and other essential oils. The best results are achieved with complete foot skin care, including the use of the main preparation at night, special tonics or lotions in the morning and foot baths 1-2 times a week.
Foot care at home should include mechanical removal of rough skin with pumice stones of varying hardness. Daily use of pumice allows you to remove regrown skin in a timely manner. To prevent hyperkeratosis, just a few movements of the pumice stone over the entire surface of the foot are enough. Before using pumice, you must first wash your feet, but do not dry them, because pumice “loves” damp skin surfaces.
By following these simple rules for home foot care, you can prevent the development of hyperkeratosis or significantly alleviate it.
Treatment in the pediatrician's office
Hyperkeratosis of the foot is treated by an orthopedic surgeon with a medical education. The treatment plan is based on many years of experience and includes several stages: softening the rough skin of the feet, removing the hard stratum corneum and regenerating the skin.
There are several ways to soften the hard stratum corneum. The classic method uses water as a softener and sometimes adds salt or spices - it's economical and fun. In modern cosmetology, chemical emollients in the form of solutions, gels or foaming agents are increasingly used. Their undeniable advantages are a good disinfecting effect, cost-effectiveness and efficiency.
Removing iron ore using disposable tools: a scalpel and a removable blade of various sizes.
Areas of hyperkeratosis on the soles of the feet, toes, or metatarsophalangeal joints resemble narrow strips or grains of rice. Use a hollow knife to successfully remove hard skin in these areas.
The podiatrist very carefully removes the hardened layer of skin with strict vision, which is even worse for young pink skin. When performing technically correct procedures without violating the integrity of soft tissues, the hard stratum corneum is removed without a trace.
The final step in treating hyperkeratosis podiatry is skin rejuvenation. This can be done using traditional files and hardware methods using disposable ceramic tips. The technical pedicure technology has advantages in terms of speed, hygiene and greater efficiency.
Classification, reasons
Keratosis comes in different types. The most common:
- follicular;
- actinic;
- seborrheic.
The causes of some keratoses are not always clear and not fully understood, but factors contributing to their development have been identified. The impetus for the formation of keratosis pilaris in children and adults is:
- the effect of cold on the skin;
- lack of vitamins A, C and D;
- long-term use of hormonal drugs;
- improper mode of work, rest, sleep, nutrition;
- regular stress and nervous exhaustion.
Actinic keratosis is also called solar keratosis or senile acanthoma. Its cause is the action of direct sunlight.
Theories have been put forward that the impetus for the development of seborrheic keratosis is the following factors:
- human papillomavirus;
- action of ultraviolet rays;
- burdened heredity - the disease is more common in families where one of the family members has already experienced the described pathology.
Seborrheic keratosis is mainly observed in old age.
Types of hyperkeratosis and causes of its appearance
Depending on the origin, the disease is divided into acquired and hereditary. Based on the nature of the manifestation, the following forms of hyperkeratosis are distinguished:
- follicular;
- seborrheic;
- diffuse;
- lenticular;
- warty;
- disseminated;
- polymorphic;
- hyperkeratosis of the feet.
External factors for the development of hyperkeratosis include wearing tight and constricting clothing and shoes, frequent contact with chemicals (professional costs), and failure to comply with personal hygiene rules. Internal causes of hyperkeratosis include various skin diseases, including:
- ichthyosis;
- seborrheic dermatitis;
- lichen;
- psoriasis;
- foot fungus;
- disruption of keratin production;
- keratoderma.
Some causes of the disease include endocrine diseases, including diabetes mellitus, excess body weight, vitamin deficiency and erythroderma.
Symptoms
A symptom of keratosis pilaris is a skin condition that can be described as “chicken skin.” Small, hard, light-colored irregularities form. They can occur on the upper arms, thighs, and less commonly on the face.
Actinic keratoses appear as patches on the head, neck, or arms. Their characteristics:
- by color - red, brown, flesh-colored;
- in size - mostly 1-3 mm in diameter;
- texture – rough;
- surrounded by red skin.
Seborrheic keratosis (including facial keratosis) appears as growths on the skin:
- round or oval;
- flat or slightly protruding above the surface of the skin;
- in size - from 0.2 to 2.5 cm in diameter;
- in color - from light brown to black.
For what reasons do acquired keratoses occur?
The main cause of almost all keratoses is said to be chronic exposure to ultraviolet rays. In the literature, all changes associated with sun exposure are often grouped under the term dermatoheliosis. Thus, the damaging effect can affect the epidermis (senile, actinic keratosis), dermis (solar elastosis), blood vessels (telangiectasia), sebaceous glands (porokeratosis) and melanocytes (dyschromia).
The effects of sun damage to the skin gradually accumulate as the total amount of time spent exposed to UV rays increases year after year. This leads to the fact that the peak incidence of this nosology occurs at the age of 50 years and older.
However, nowadays, actinic keratosis has become much more common in young people. As a rule, these are people of the first and second phototypes (with fair skin, blond or red hair, and blue, green or gray eyes). There is a high likelihood of developing keratoses in young people exposed to sunlight for a long time.
The incidence is slightly higher in men because they tend to use little or no sun protection. Clinical studies estimate that about 60 percent of predisposed individuals by the age of forty have at least one element of actinic keratosis. Some experts believe that almost everyone over the age of 80 suffers from some form of keratoses.
In addition, persons whose immune defenses are weakened by chemotherapy, extensive exposure to x-rays or a number of industrial chemicals, patients with AIDS, patients who have undergone organ transplants, patients with disorders of the nervous and endocrine systems, etc. less able to combat the effects of radiation and, therefore, more prone to developing keratoses.
Keratosis: diagnosis
Keratosis is detected based on examination of the skin using a magnifying glass and a light source. Anamnesis (history of the disease) is important - the doctor clarifies the following nuances of the pathology:
- presence in the family of people with keratosis;
- connection with solar radiation;
- mode of work and rest.
The patient’s age is also taken into account – this applies to the diagnosis of seborrheic (senile) keratosis.
Additional research methods (instrumental and laboratory) are required if it is necessary to differentiate keratosis from other diseases - for example, from skin cancer, when it is necessary to involve a biopsy (sampling of skin fragments followed by examination under a microscope).
Diagnosis and treatment of the disease
If characteristic skin problems appear, you should consult a dermatologist as soon as possible. The specialist examines the skin and collects the patient’s complaints. It is important to differentiate hyperkeratosis from other skin diseases, for example, psoriasis or lichen, which also cause peeling of the skin. If the diagnosis is in doubt, a biopsy of suspicious skin areas may be performed.
To treat the disease, ointments with topical corticosteroids are used to treat the damaged areas. This may include prednisolone or hydrocortisone ointment, fluacinolone-based formulations, or clobetasol. In addition, glucocorticoid drugs are prescribed, which have an exfoliating and anti-inflammatory effect, thoroughly cleansing and disinfecting the skin.
Patients with hyperkeratosis of any form are advised to take warm baths with the addition of salt, baking soda or starch and further moisturizing with cosmetic creams.
If hyperkeratosis is detected, mechanical peeling is contraindicated, as it can aggravate the patient’s condition. Only acid (chemical) peeling based on creams with a mild effect is allowed. These are products consisting of salicylic, lactic, citric and other acids. Vitamins A and C are also prescribed orally.
Plantar hyperkeratosis is treated with antifungal ointments, and also requires the elimination of all pathological factors of the disease. It is necessary to replace shoes with more comfortable ones, as well as receive orthopedic help in case of flat feet or club feet. In addition, salt baths, mechanical grinding using a hard sponge and pumice at home are useful. After this, the feet are lubricated with a moisturizing and nourishing cream.
As for possible complications of the disease, they can be observed with plantar hyperkeratosis, when cracks, corns appear, and a secondary fungal infection begins to develop. Follicular hyperkeratosis in some cases causes pyoderma. Formations with a warty form sometimes develop into a malignant tumor. The prognosis for timely and high-quality treatment of hyperkeratosis is favorable, although in some cases the fight against the disease can last a lifetime with alternating stages of exacerbation and remission.
Keratosis: treatment
Signs of keratosis pilaris often disappear on their own. If this does not happen, the doctor will prescribe products that help remove dead skin cells. They contain:
- alpha hydroxyl acids;
- lactic acid;
- retinoids.
Does keratosis pilaris leave marks on the skin? Treatment includes the use of moisturizing creams to improve the appearance of the affected areas.
If actinic keratosis develops, the doctor recommends avoiding exposure to sunlight.
Of all the keratoses, actinic keratosis is the most dangerous: treatment may require surgical removal of the affected areas of the skin, as this type is prone to turning into cancer. Such areas are eliminated using different methods - this can be:
- cryotherapy – exposure to liquid nitrogen;
- curettage - cleaning the skin by scraping with a curette (a spoon with sharp edges);
- laser resurfacing.
Seborrheic keratosis is less dangerous - treatment includes treatment with the following substances:
- ammonium lactate;
- trichloroacetic acid;
- some creams with an abrasive (scraping) effect.
Doctor Komarovsky's opinion
Before you begin to treat the disease, you need to find out why it appeared , and only then take any action.
In some cases, the disease goes away on its own , however, sometimes the child still requires adequate therapy.
You should not self-medicate, since children's skin is very sensitive to the effects of many medications that can cause serious irritation. Therefore, only a doctor should prescribe therapy.
Prevention
There are no special methods for preventing keratosis pilaris. To reduce the risk of its occurrence, the following are relevant:
- relief of skin irritation;
- increasing the body's immune forces.
If you take precautions, treatment of keratosis if it occurs will be more successful.
The method of preventing actinic keratosis is to avoid exposure to direct sunlight. The risk of developing seborrheic keratosis can be reduced if you take proper care of your skin throughout your life - thanks to this, the aging process of the skin will occur later.
General recommendations for the development of any type of keratosis are to follow a healthy lifestyle and avoid prolonged exposure to UV rays on the skin.
On our website Dobrobut.com you can get more detailed information about how keratosis occurs, what it is, and how to treat it.
Localization of the lesion
Characteristic manifestations of keratosis pilaris can occur on almost any part of the body where there is hair (hair follicles).
Thus, nodular formations can affect the area of the face and arms (this happens most often), as well as the hips, buttocks and legs, the area between the shoulder blades and the chest.
On the inside of the palm and on the skin of the feet, these changes practically do not occur (with the exception of some forms of the disease), since there are no hair follicles in these areas.
Are there possible complications and consequences?
Follicular keratosis, not accompanied by other diseases, does not pose any threat to the child’s health. Pathology only causes psychological discomfort due to its external manifestations.
The disease proceeds without complications and does not have a negative effect on the child’s internal organs.
The risk lies in scratching the affected areas and mechanical damage to the skin when itching occurs. Through the resulting wounds, a bacterial infection can occur, which will lead to the formation of foci of purulent inflammation of varying severity.
What kind of disease is keratosis pilaris?
Follicular keratosis is a common dermatological disease associated with disruption of the normal processes in the upper layers of the epidermis.
It is seasonal in nature, since its symptoms most often appear in winter, which most experts associate with vitamin D deficiency in the cold season.
Signs of the disease often appear in childhood and are expressed only in external manifestations. In most cases, after puberty, symptoms go away on their own without any additional therapy.