Bartholinitis is an inflammation of the large Bartholin gland. The Bartholin gland, in turn, is a paired organ that is located in the subcutaneous fatty tissue of the labia majora. When a large gland in the vestibule of the vagina becomes inflamed, microorganisms affect the excretory duct of the gland (canaliculitis), as well as the gland itself.
The main function of the Bartholin gland is to produce secretions that maintain constant moisture in the vagina. What is it for?
This secretion is released in large quantities during arousal during sexual intercourse to facilitate penile insertion. In addition, secretion is very important during childbirth. Thanks to it, the vaginal muscles stretch well and the baby can be born without damaging the vaginal walls. If the Bartholin gland does not produce secretions in the required quantity, the vagina will become dry - discomfort, itching and burning in the perineum and pain during sexual intercourse will appear. Normally, this is only possible during menopause due to the age-related decrease in female estrogen hormones.
Causes of bartholinitis:
Bartholinitis occurs due to infection in the Bartholin gland through a narrow opening of the excretory duct on the inner surface of the labia minora. Once deep into the gland, microorganisms actively multiply. This leads to inflammation and suppuration of the Bartholin gland.
Not all genitourinary infections cause bartholinitis. In the vast majority of cases, bartholinitis is provoked by sexually transmitted infections. Most often it is gonorrhea, less often - trichomoniasis and chlamydia.
Bartholinitis of nonspecific etiology is extremely rare - in this case, the causative agent is bacteria - staphylococci, Escherichia coli, streptococci, and so on. This is possible if personal hygiene rules are not followed. It should also be taken into account that even in the presence of sexually transmitted infections, bartholinitis does not develop in everyone and not always.
Immunity plays an important role in the development of the disease: if it is weakened, the chances of developing bartholinitis increase.
Depending on the clinical course of the disease, bartholinitis can be acute or chronic. Acute bartholinitis is characterized by the formation of a true or false abscess of the Bartholin gland (a limited focus with pus).
When a false abscess forms, the excretory duct of the gland first becomes inflamed (“canaliculitis”, in scientific terms). The skin over the site of inflammation turns red and swells. If you press on the inflamed area, pus will come out. Next, a blockage of the excretory duct of the gland occurs and pus is no longer released, but accumulates in the Bartholin gland. Because of this, the gland is greatly stretched and protrudes, forming a painful “bump”-shaped formation. During movements - when walking, running, during sexual intercourse - the pain intensifies, and a burning sensation appears in the perineum. Sometimes body temperature rises slightly. If you do not contact a gynecologist for a long time, the disease becomes chronic.
With a true abscess, the infection penetrates directly into the Bartholin gland, and the parenchyma of the gland melts. In this case, the symptoms of the disease are more pronounced than with a false abscess. The labia majora and minora become very swollen. The body temperature rises to more than 38 degrees, the inguinal lymph nodes enlarge, chills, weakness, and “pulsating” sharp pain in the labia majora appear. Spontaneous opening of the abscess with the release of yellow-green pus is possible, which leads to a weakening of the symptoms of the disease. But if left untreated, the inflammation recurs again and gives complications, or, like a false abscess, becomes chronic.
In the chronic form of bartholinitis, the symptoms of the disease temporarily subside and worsen again. Instead of an abscess, a cyst (liquid formation with inflammatory exudate) forms in the gland.
With any form of bartholinitis, you should never self-medicate or try to squeeze out an abscess or cyst - this can lead to blood poisoning . If such symptoms occur, you should immediately consult a gynecologist.
1. Lipomas
Formations on the genitals come in several varieties. The reasons, patterns, mechanisms of their occurrence in some cases are known and understandable, in others they remain not entirely clear. Different types of formations affect specific tissues. The following types of formations on the external genitalia are divided: lipoma, atheroma, bartholinitis, papilloma.
Lipomas
most often form in the subcutaneous fat layer. It is impossible to clearly identify the reasons for their occurrence, but a certain statistical connection with hereditary predisposition has been established. Moreover, the growth of lipomas has nothing to do with fat consumption or a tendency to develop subcutaneous fat deposits. The incidence of lipomas in thin and overweight people is the same. Lipomas can range in size from 1 to 15 cm and are usually not painful or itchy, presenting only a cosmetic problem. Cases of malignant degeneration of lipomas are very rare; More often, mechanical damage carries the threat of suppuration and infection. Lipomas up to 3 cm are treated non-surgically - by injecting them with a drug, the action of which leads to the resorption of the formation. Large lipomas are removed surgically: with laser, electrocoagulation or radioknife.
As a rule, a new lipoma does not appear at the site of a well-performed operation. However, it is not uncommon for new lipomas to form in nearby tissues.
A must read! Help with treatment and hospitalization!
Diagnosis of bartholinitis:
Diagnosing bartholinitis is not particularly difficult. The doctor will be able to make a diagnosis during examination at the first appointment. In the presence of an abscess, swelling and redness of the Bartholin gland is determined; palpation of the formation causes sharp pain. In the chronic form of bartholinitis (in the presence of a Bartholin gland cyst), a tumor-like formation is detected, painless on palpation. In addition to the examination, the following tests must be taken:
- a regular vaginal smear;
- PCR diagnosis of major sexually transmitted infections (chlamydia, gonorrhea, trichomoniasis, mycoplasmosis, ureaplasmosis, herpes, human papillomavirus);
- bacteriological culture of vaginal discharge to establish sensitivity to anitibiotics;
- bacteriological examination of pus when an abscess ruptures (or the secretion can be obtained from the excretory duct of the gland by light pressure).
Inflammation of the labia in women, video
Gynecologist Irina Vladimirovna Garyaeva about vulvitis in women.
Source - KVD - dermatovenerological dispensary Sources:
- ROLE OF INFECTIONS IN THE GENESIS OF VULVA DISEASES. Reutskaya M.A., Kulinich S.I. // Siberian Medical Journal (Irkutsk). – 2010. – No. 6. – pp. 239-242.
- CLINICAL AND MORPHOLOGICAL PRINCIPLES OF TREATMENT OF CHRONIC VULVITIS. Kulinich S.I., Reutskaya M.A., Pokinchereda T.V., Ezhova I.V. // Acta Biomedica Scientifica. – 2013. – No. 5 (93). – P.42-48.
- Diseases of the cervix, vagina and vulva: Clinical lectures. Ed. V.N. Prilepskaya. // M.: MEDpress. - 1999. - P. 432.
- Recurrent vulvovaginal candidiasis: etiology, pathogenesis, treatment. Levonchuk E.A. // Med. news. - 2001. - No. 4. — P. 40-43.
- Dystrophic diseases of the vulva. Diseases of the cervix, vagina and vulva. Ed. V.N. Prilepskaya. // M.: MEDpress. - 1999. - pp. 326-336.
- https://simptom-lechenie.ru/en/vulvit-u-zhenshhin-i-devochek-simptomy-i-lechenie.html
- https://www.thenakedscientists.com/science-articles
- https://woman-centre.com/vlagalische-i-vulva/vulvit/vulvit-u-zhenshhin.html
- https://simptomer.ru/bolezni/zhenskie-zabolevaniya/864-vulvit-simptomy
Surgical treatment of Bartholin gland cyst:
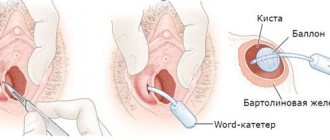
Treatment of Bartholin gland cysts is carried out without exacerbation of the inflammatory process. In this case, there are two options for surgical intervention: marsupialization of the cyst (creation of an artificial duct of the gland for the outflow of secretions) or extirpation (removal) of the Bartholin gland.
When performing marsupilization, the doctor opens the cyst capsule with a linear incision. The edges of the capsule are sutured with separate sutures to the edges of the skin wound, forming an external opening. A drainage tube or catheter is inserted to drain the contents of the cyst. After the operation, within two months, the external opening narrows, and a new excretory duct is formed.
Extirpation of the gland is carried out in case of recurrence of bartholinitis. To do this, a longitudinal incision is made on the inside of the labia minora. The gland is carefully isolated with a scalpel and removed, and catgut sutures are placed on the wound.
For any types of bartholinitis, after surgery and complete elimination of the inflammatory process, physiotherapy is prescribed on the 3-4th day - magnetic therapy and ultraviolet irradiation. All patients are advised to abstain from sexual intercourse until complete recovery, since there is a high probability of infection of the sexual partner. In order to prevent a relapse of bartholinitis, it is important to eliminate the cause of the disease, to completely recover from concomitant infections (chlamydia, gonorrhea, etc.), otherwise bartholinitis may occur again.
All patients must observe the following rules of personal hygiene:
- wash your face twice a day;
- wear comfortable underwear, preferably cotton;
- During menstruation, change pads and tampons every 3-4 hours to avoid re-infection.
During the recovery period, it is important to use drugs that enhance the immune system. These include vitamins, a balanced diet, and some herbal immunomodulators.
2.Atheromas
Atheroma
is a cyst filled with a yellowish fluid formed by fat cells, epidermis and sebum. Since all this in the cyst is in a state of stagnation, when opened, the substance that is usually removed has an unpleasant odor. Causes of atheroma: increased oily skin, acne, poor cleanliness, hormonal changes, heredity. Atheromas form where there are many sebaceous and sweat glands. When they grow to a size of 5 cm, tension occurs on the surface of the skin and even internal inflammation is possible. It is always recommended to remove atheromas without waiting for complications, although they also degenerate extremely rarely.
The atheroma is completely removed by isolating it from the tissue. At the same time, they try not to disrupt its integrity and make sure that no particles of the cyst shell remain, otherwise this may cause a relapse in the same place.
Visit our Gynecology page
Prevention of bartholinitis:
- regular visits to the gynecologist;
- protection against sexually transmitted infections - use of condoms, monogamous lifestyle;
- timely treatment of infections;
- strengthening the immune system: good nutrition, exercise, giving up bad habits.
In our clinic you can receive a full range of clinical and laboratory examinations before performing this surgical operation. The equipped operating room allows you to perform the operation both under local anesthesia and general anesthesia, with stay and observation in the ward for several hours.
Warts, papillomas
Papillomas are located on the labia, warts on the mucous membrane at the entrance to the vagina and entrance. Both neoplasms are flesh-colored and do not differ in any way from the skin; in fact, this is the skin, the growing epidermis. For the experienced eye of a gynecologist, it is not difficult to determine the skin that has changes. Formations can look different: in the form of grapes, peas, fringes, so-called cauliflower and other associations. What unites them all is a small attachment point, in the form of a leg, through which nutrition flows through the vessels and the formation grows.
Condylomas can be solitary or localized in groups, subsequently merging.
When rubbed with clothing, during sexual intercourse, hygiene procedures, the formations are damaged, which contributes to even greater growth and penetration into the urethra, vagina, uterus, and anus.
Therefore, it is necessary to remove condylomas on the genitals as soon as possible after detection.
Removal of papillomas on the labia
Removal of genital papillomas has long become a fairly common procedure that reduces the risk of developing cancer.
After the results of the examination of the tumor are received, the gynecologist determines treatment for each patient. The most effective method of removal is radio wave. It is advantageous in that it does not damage nearby healthy tissue, causes minimal discomfort and has a minimal cauterization site.
For maximum effect, rapid healing and cure of papillomatosis, removal is combined with immunomodulatory and antiviral therapy. This increases the chances of preventing the recurrence of formations.
Survey
It is enough for a specialist to establish a diagnosis by palpation of the node, without additional research. The existence of an excretory duct, which is the main sign in the diagnosis of atheroma.
The inflammatory process can be an obstacle to an accurate diagnosis. Unfortunately, women come to us at the most critical moments of this disease, when the inflammatory process progresses.
To be on the safe side, doctors often carry out an additional check to ensure that the nodule is benign.
What symptoms do you see a surgeon for:
- Presence of hernial protrusion
- Daggering pains in the abdomen
- Bloating
- Pain in the right hypochondrium
- Bitterness in the mouth
- Nausea
- Presence of neoplasms on the skin
- Swelling and redness of the skin
- Bone fractures and bruises
- Wounds of any location
- Vomit
- Enlarged and painful lymph nodes