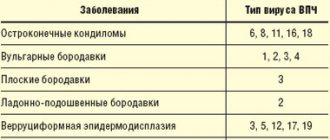
Genital warts in women (syn. - intimate papillomas, PVI, genital warts, venereal condylomatosis) are a group of viral infectious diseases characterized by the development of papillomatous formations on the skin and mucous membranes of intimate places.
Condylomas in gynecology are classified as diseases transmitted sexually, as well as through contact and household contact. Infection usually occurs during sex in the vagina, rectum, and less commonly through oral contact. A regular condom often does not become a barrier to HPV, since the size of the virus is much smaller than the size of the condom pore. HPV can only be transmitted from person to person. Self-propagation of formations throughout the body with the emergence of new foci is possible. In 50-70% of children born to infected mothers, vertical transmission of papillomavirus occurs.
HPV can persist for a certain time in exfoliating epithelial cells - therefore, for some diseases caused by this virus, a household route of infection (warts, intimate condylomas) is also likely, especially if there are microdamages to the skin. The widespread belief that these warts of the urogenital zone of any location can only be found in people who are sexually active or practicing other forms of intimate relationships is erroneous - they are often found in the intimate places of absolute virgins, children and teenage girls of different ages.
HSV and HPV: similarities and differences
First of all, it is important to understand that the herpes simplex virus (HSV) and the human papillomavirus (HPV), which provoke herpes and human papillomavirus infections, respectively, are fundamentally different from each other.
"Galavit" for herpes virus infection helps:
- Pronounced elimination of viruses from the body
- Increasing the effectiveness of antiviral therapy
- Reducing the period of rashes and accelerating regeneration processes
- Increased duration of remission
In adults and adolescents over 12 years of age in complex therapy:
Suppositories
- 5 days, 1 suppository, then one every other day. Course - 2 packs of suppositories.
Sublingual tablets
— 10 days, 1 tablet 4 times a day. Then continue taking it every other day for 10 days, 4 tablets per day.
THERE ARE CONTRAINDICATIONS. YOU SHOULD CONSULT WITH A SPECIALIST.
HSV
Genital herpes is associated with infection with HSV type 1 or 2. According to statistics, the disease affects about 12% of the population [1]. Once it has penetrated the body, the virus “settles” in it forever - today there is no treatment method for the herpes virus that would allow one to finally get rid of the pathogen. Symptoms of genital herpes, which occur periodically during relapses, significantly reduce the quality of life. Interestingly, the frequency of new episodes of the disease depends on the type of virus: with HSV-1 infection, approximately 1 relapse is recorded per year, while with HSV-2 infection, their number can reach 6 or more [2].
Despite the fact that there is no specific treatment for HSV, a number of drugs can alleviate the condition during exacerbations. According to domestic and Western recommendations, oral antiviral agents for herpes based on acyclovir and valacyclovir are used for this purpose. However, in Russia local therapy is also recommended, which is not included in Western standards. Abroad, such methods are not included in the recommendations due to their lower activity compared to tablets [3].
HPV
The situation with papillomavirus infection (HPV) is somewhat different. It is considered the most common sexually transmitted disease in the world [4]. Most adults become infected with HPV at some point in their lives, but in 90% of cases the virus clears naturally within two years of infection. Otherwise, the infected person becomes a lifelong carrier.
Unfortunately, there is no cure for the human papillomavirus, just as there is no cure for the herpes simplex virus. However, the first, unlike the second, can be deadly: HPV types 16 and 18 are associated with malignant neoplasms - in particular, cervical cancer and some other tumors. The only effective drug treatment for human papillomavirus infection today is the eradication of condylomas, which are manifestations of clinical and subclinical forms of infection. For this purpose, a number of local antiviral drugs that have proven activity in studies are used in the treatment of human papillomavirus. At the same time, in domestic practice, doctors also prescribe drugs that have a dubious evidence base. Let's look at their advantages and disadvantages in more detail.
Causes
Condylomas in men and women can appear due to the following reasons:
- unprotected sexual intercourse;
- decreased immune defense in acute respiratory infections or acute respiratory viral infections;
- general use of personal hygiene items and products;
- oral or anal sex;
- stress;
- vaginal dysbiosis;
- decreased immunity due to HIV or syphilis;
- endometritis or endometriosis;
- pregnancy and decreased protective functions in the body;
- taking glucocorticoid drugs.
Local immunomodulators for HPV and HSV
Among the “universal” drugs that can be prescribed for various viral infections - from common respiratory infections to herpes and human papillomavirus - are interferons. In particular, preparations of human recombinant interferon alpha-2b.
Interferon alpha-2b has antiviral, immunomodulatory and antiproliferative properties. It suppresses the replication of RNA and DNA viruses, enhances the activity of macrophages, and increases the cytotoxicity of lymphocytes to target cells. The use of drugs containing interferon alpha-2b is accompanied by an increase in the level of immunoglobulins type A and normalization of IgE [5]. However, these therapeutic effects are fully manifested when the drug is administered systemically.
when its high concentration in the blood is reached. It should be noted that quite powerful side effects can develop, including fever, loss of appetite, headaches, muscle pain, joint pain and many other adverse reactions.
Due to the specific safety profile, injectable interferon preparations are prescribed only in very serious cases, when the risk of side effects is justified - for example, in the treatment of hepatitis, a number of oncological diseases, etc. HSV and HPV infections do not apply to such situations and are not indications for systemic interferon administration. At the same time, the Russian Federation has registered a very impressive list of local forms of interferon alpha-2b, including ointments/creams for treating mucous membranes with genital herpes.
Theoretically, local interferon preparations should have all the advantages of injectable ones and not have their side effects, since local forms are either very slightly absorbed into the systemic circulation or do not penetrate into the blood at all. However, today there is no sufficiently reliable evidence of the effectiveness of interferons when applied topically. However, in domestic practice they are quite often prescribed as part of the complex treatment of recurrent genital herpetic infections.
Along with local forms containing only interferon alpha-2b, several combination drugs are also registered in the Russian Federation:
- Interferon alpha-2b + acyclovir + lidocaine, ointment. Indications: HSV.
- Interferon alpha-2b + taurine + benzocaine, vaginal and rectal suppositories, prescription. Indications: HSV, HPV. Taurine, according to the instructions, acts in combination as a reparative, antioxidant and anti-inflammatory component.
+
High safety profile.
!
The feasibility of using local forms of acyclovir for genital herpes is subject to serious doubts due to insufficient activity, which is confirmed in Western recommendations [3]. Interferon alpha-2b preparations, both mono- and combined, are available with or without a prescription, depending on the indications of the dispensing rules in the instructions for a particular drug. It is important to draw the visitor’s attention to the fact that the first-line treatment for HPV - oral forms of acyclovir and valacyclovir - must be prescribed by a doctor, so you should be advised to immediately consult a doctor.
When to see a doctor
If you begin to notice pointed bulges on your body that were definitely not observed before, we recommend that you immediately contact a specialist. You should not wait until the disease begins to cause complications. Removal of genital warts is recommended to take care of health and maintain aesthetic beauty. For example, burning out a tumor with a laser is one of the fastest and most effective methods. The procedure takes a few minutes. The patient may only feel a slight burning sensation, a feeling of warmth. The procedure is not accompanied by pain or severe discomfort. It is not hazardous to health. The laser beam hits a precisely targeted target. Healthy tissues are not affected. Therefore, laser cauterization does not leave scars or stains. A small brown spot then forms at the site of the condyloma. The dermis will heal within 5-10 days. A crust will appear on the surface that cannot be picked or scratched. It provides protection against bacteria and infection.
As soon as the site of the removed condyloma heals, the crust will fall off on its own. Immediately after the procedure, you should not take a bath, visit the sauna, pool, or be in the open sun. All water procedures are acceptable after 5-7 days.
You can receive complex treatment at JSC "Medicine" (clinic of Academician Roitberg) in the center of Moscow at the address: Mayakovskaya metro station, 2nd Tverskoy-Yamskaya lane, building 10. Leading specialists work here, who select an individual approach for each patient, taking into account characteristics of his illness.
Synthetic antiviral topical drugs
This group of drugs can be roughly divided into drugs used for genital herpes infection and antiviral drugs prescribed for the treatment of papillomas and condylomas associated with papillomavirus infection.
Local medications for genital herpes
Several drugs registered in the Russian Federation are used for the treatment and prevention of relapses of genital herpes.
Tromantadine
An antiviral drug for herpes, an adamantane derivative (similar to the well-known antiviral drugs rimantadine and amantadine). Inhibits the attachment of the virus to the surface of the cell membrane, preventing the pathogen from penetrating into the cell. Prevents cell fusion and makes it difficult for the virus to spread by changing the synthesis of glycoproteins [5]. Available in the form of a gel for external use, which can be applied to mucous membranes during exacerbation of HSV infection [5].
Vacation: without prescription.
!
There is evidence of the development of a contact allergic reaction when using the drug [7].
Sodium aminodihydrophthalazindione
An immunomodulator capable of regulating the activity of innate and acquired immune cells, including macrophages, neutrophils and natural killer cells. At the same time, this antiviral drug against herpes increases the body's resistance to bacterial, viral and fungal infections, reducing their frequency, severity and duration (5). In addition, the drug normalizes the formation of antibodies and regulates the production of interferons, and also blocks the excessive synthesis of pro-inflammatory cytokines and reduces the level of oxidative stress (5).
Vacation: Without prescription
+
High safety profile (5).
Azoximer bromide
A Russian drug supposedly exhibiting an immunostimulating effect. According to the instructions [5], it directly affects phagocytes and natural killer cells, stimulates the formation of antibodies and the synthesis of interferon, and exhibits antioxidant and detoxifying properties. In domestic practice, it is used for a wide range of diseases - from influenza to malignant neoplasms.
Azoximer bromide vaginal suppositories are used to prevent recurrence of genital herpes.
Vacation: without prescription.
+
High safety profile. According to the manufacturer [5], no side effects have been reported.
!
Azoximer bromide suppositories are not indicated for the treatment of active herpes!
Diagnosis of genital warts
Typically, diagnosing skin growths in intimate areas is not difficult. A doctor can visually identify condylomas. If several neoplasms grow and merge into a single focus, a characteristic colony is formed. It looks like cauliflower.
To accurately confirm the type of pathogen and exclude a malignant process, the following additional studies are carried out:
- colposcopy;
- PCR diagnostics;
- cytological screening;
- biopsy.
Before deciding to remove condyloma, it is important to exclude the possibility of the presence of atypical (malignant) cells.
Topical antiviral drugs for the treatment of HPV (papillomavirus)
Some topical antiviral drugs active against papillomaviruses, in contrast to a number of drugs that help against the herpes virus, have a strong evidence base and are used throughout the world to treat manifestations of HPV - in particular, condylomas.
Imiquimod
An immune response modifier that does not have an antiviral effect. It exhibits activity due to the ability to induce the production of interferon-alpha and other cytokines. Indicated for the treatment of genital warts in the urogenital area [5].
Release: by prescription.
+
Solid evidence base. The drug definitely reduces the viral load. The use of imiquimod cream 5% 3 times a week at night for 16 weeks has been proven to be effective and safe for the treatment of condylomas. The relapse rate is estimated to be low [8]. Imiquimod is recommended for the treatment of genital warts by the authoritative American regulator FDA [8].
!
When applying imiquimod, itching and pain are observed in more than 10% of cases [5], which the buyer should be warned about.
Complications
Condylomas themselves on the head, labia or other surfaces of the body are not as dangerous as complications after them. The infection rate is 80-90%.
The proliferation of genital warts can lead to:
- the addition of a secondary infection (suppuration, inflammation);
- fusion of the foreskin;
- malignant tumors.
Therefore, it is impossible to postpone the removal of condylomas with a laser or other method. It is necessary to eliminate not only the warts themselves, but also to comprehensively strengthen the immune defense of your body.
Local antiviral herbal remedies
Ammonium glycyrrhizinate
The active component of the drug, activated glycyrrhizic acid, is obtained from licorice root. It has a complex immunostimulating, antiviral, anti-inflammatory, antipruritic effect. Glycyrrhizic acid interrupts the replication of a number of DNA and RNA viruses, including herpes simplex virus, human papillomavirus, and cytomegalovirus [5].
Indicated as a drug for the treatment of human papillomavirus infection and herpes simplex virus, including infection with oncogenic viruses. Available in the form of a spray, which is sprayed onto the mucous membranes and affected areas of the skin.
Vacation: without prescription.
+
It has a wide range of indications, including the prevention and treatment of vulvovaginal candidiasis, discomfort in the genital area. Can be used during pregnancy and breastfeeding; well tolerated.
Podophyllotoxin
The active component of podophyllin, a derivative of plant extracts isolated from the rhizomes with roots of Podophyllum thyroid - a plant of the barberry family. It has pronounced antitumor and antiviral properties and has a cytotoxic effect. When used externally, it cauterizes and mummifies condylomas. It is used as a drug for local treatment of human papillomavirus. Available in the form of a solution for the treatment of genital warts [8].
Release: by prescription.
+
Proven effect. According to research, a 0.5% solution of podophyllotoxin reduces the number of anogenital warts from 6.3 to 1.1, destroying about 70% of formations [8].
!
Care must be taken when using - contact with healthy skin can lead to ulceration. Local reactions during use, allergic reactions. The physician, when dispensing this antiviral drug for papillomas and condylomas, must draw the client’s attention to this feature and remind him that the drug should be stored out of the reach of children.
Tetrahydroxyglucopyranosylxanthene
Russian drug. The active component is isolated from the Alpine kopek plant or the yellow kopek plant.
According to the instructions, it has antiviral activity against HSV-1 and HSV-2, as well as cytomegalovirus and some other DNA-containing viruses. In addition, the drug presumably activates cellular and humoral immunity, inhibits the growth of a number of bacteria and pathogenic protozoa, including Trichomonas, and also has a moderate anti-inflammatory effect. Used in the form of an ointment as part of the combined treatment of acute and recurrent forms of herpes, including genital herpes [5].
Vacation: without prescription.
+
Favorable safety profile, the ability to be used as part of complex treatment.
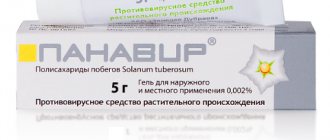
Polysaccharides of Solanum tuberosum shoots
A Russian prescription drug, the active component is obtained from the shoots of tuberous nightshade. According to the instructions, it exhibits an antiviral effect against HSV-1 and HSV-2, promotes the induction of interferons and increases the immune response [5]. It should be noted that the pharmacokinetic properties of the drug have not been studied. Vaginal suppositories are used in complex therapy of genital herpes.
Vacation: without prescription.
+
High safety profile. Side effects are rare.
Desmodium canada herb extract
An antiviral drug for herpes of plant origin, created from a dry extract of the herb Desmodium canadensis. According to the instructions, it exhibits antiviral activity against herpes viruses and stimulates the production of interferon [5]. The ointment is indicated for use in acute and recurrent forms of herpes, including urogenital.
Vacation: without prescription.
+
High safety profile - no side effects identified.
Hyporamine extract
Russian development based on sea buckthorn leaf extract. According to the instructions, it is active against herpes simplex viruses, cytomegaloviruses and some others [5]. An ointment containing hyporamin extract is indicated for the treatment and prevention of episodes of herpes, including genital herpes.
Vacation: without prescription.
+
High safety profile; Possibility of use during pregnancy and lactation (after consultation with a doctor).
Laser removal
This is a modern method of excision of formation, which has become widespread.
Its popularity is due to its advantages:
- painlessness;
- low-injury;
- bloodlessness;
- speed of the procedure;
- minimal risk of infection;
- short rehabilitation period;
- no scars.
Thanks to the precision of the laser beam, it is possible to remove growths even in particularly sensitive areas, such as the intimate area, eyelid, etc.