Molecular biological methods for diagnosing HPV infection
Cervical cancer is preceded for several years by precancerous lesions, which are called CIN-cervical intraepithelial neoplasia of three degrees. CIN I is not precancerous and has a high degree of regression, however, in the presence of the HPV virus, CIN is highly likely to develop into CIN II and CIN III, true precancerous lesions. There is a wide range of methods for diagnosing cervical cancer and precancerous lesions:
- clinical;
- cytological (Pap-test);
- extended colposcopy;
- determination of HPV DNA using real-time PCR;
- determination of HPV viral load using the Digene test;
- liquid-based cytology;
- morphological study;
- tumor markers: determination of oncoproteins p16, ki67, mcm2, mcm7, Hsp27, etc.;
- real-time cervical scanning (TruScreen).
HPV DNA testing is a molecular biological method used in addition to cervical screening in women starting at age 30, and also as a triage test for unclear cytological results.
Molecular biological methods provide information about the development of HPV infection, but do not allow us to judge the presence of the disease, since the fact of HPV infection is not always associated with the disease. The two main methods for diagnosing HPV DNA are real-time polymerase chain reaction (PCR) and the hybrid capture method (Digine test). Both methods practically do not differ in sensitivity and specificity, however, only the Digene test is certified and approved by the FDA. Digene test
The Digene test technology is based on hybrid capture and consists of a unique method of binding viral DNA to an RNA probe, capturing the resulting hybrid with monoclonal antibodies and chemiluminescent detection of the resulting complexes.
Essentially, this is a qualitative test that is used for preventive screening for early diagnosis of cervical pathology. The test identifies 13 high-risk genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) and 5 low-risk genotypes (6, 11, 42, 43, 44).
The test is approved by the Federal Service of the Russian Federation for Surveillance in the Sphere of Health and Social Development (FSNSZSR). The Digene test detects clinically significant levels of infection with human papillomavirus, which leads to the development of cervical neoplasia. A positive test result is reported in Digine units. A negative test virtually eliminates CIN II and CIN III.
Detection of HPV DNA in high-quality format
HPV DNA persists for a long time in tissue samples, so it can be easily identified. To determine, a minimum amount of the test sample is sufficient. “Qualitative” determination of HPV DNA has controversial clinical significance, since it only indicates the presence of the virus, without allowing a prediction to be made regarding the course of the infection. In most cases, the infection clears up on its own.
Quantitative determination of the HPV virus
Quantitative HPV DNA testing is most sensitive in the early stages of human papillomavirus infection, when there are no other signs of infection. For example, cytological, clinical. The quantification method is used as a screening method, especially in national cervical cancer control programs, and also to evaluate the effectiveness of therapy.
Quantitative PCR methods aim to maximize the sensitivity of detecting viral DNA, however, direct clinical correlations do not always exist.
One of the criteria for a clinically significant infection, which is highly likely to develop into neoplasia, is the viral load. A viral load of 3 lg per 105 cells is clinically insignificant, since it is accompanied by a minimal risk of dysplasia and ends in spontaneous regression in almost 100% of cases. A viral load of more than 5 lg per 105 cells is considered increased and is associated with a high risk of developing dysplasia. A decrease in viral load by 1 lg over 6 months indicates a transient infection.
The prognostic value of viral load has not been clearly defined to date.
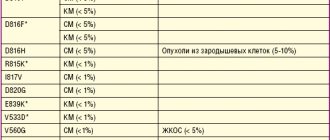
Virus genotyping
Virus genotyping using PCR allows one to determine the type of HPV virus and its oncogenicity. This method is suitable for detecting the persistence of HPV and distinguishing between cases of reinfection. Reinfection is indicated by a change in the spectrum of genotypes, while persistent infection is indicated by the persistence of the virus genotype a year after the first test.
When infected with several HPV genotypes simultaneously, the prognosis for the course of the disease is less favorable, and the risk of persistence and the risk of developing cervical cancer is higher compared to infection with one type.
Detection of high-risk HPV indicates the presence of human papillomavirus infection. Highly carcinogenic risk HPVs have different oncogenic potential. The most dangerous ones, 16 and 18, account for about 70% of all cases of cervical cancer. Genotyping for HPV 16 and 18 allows us to identify a group of women who have an increased risk of developing cervical cancer.
WHO recommendations for the prevention of cervical cancer
Methods:
- main - cytological;
- additional - DNA tests.
- Widest coverage of women.
- One-time screening of women, 35–40 years old.
- Ideal screening algorithm: 25–65 years old, initially for 2 consecutive years, with negative results every 3 years.
- The use of HPV testing will increase the intervals between screenings to 5 years.
- Using HPV testing in conjunction with the cytological method: simultaneously. HPV testing is used as the primary method. The secondary method is cytology.
Benefits of using HPV testing
- HPV testing is best used in conjunction with cytological diagnostic methods, as HPV testing has a significantly higher negative predictive value than cytology.
- HPV DNA testing provides a more interpretable result.
- To a lesser extent depends on the human factor.
- The HPV test sample is suitable for the analysis of additional molecular markers.
Genital warts
If genital warts are left untreated, they may disappear on their own, remain the same, or increase in size or number. If the warts are in the pubic area, avoid shaving or waxing as this may spread the warts. Genital warts do not cause cancer and can develop months or years after HPV infection, and they can be passed on to another person even if there are no visible signs of warts.
Cervical Cancer Screening - Key Information
HPV is a common infection and is often suppressed by natural immunity. Most types of cervical cancer can be prevented with HPV vaccination and regular screening. HPV vaccination, ideally before sexual activity, is the first line of defense and the most effective way to prevent infection. Condoms used correctly can reduce the chances of acquiring and transmitting HPV and developing diseases associated with the virus.
Causes of the disease
A virus is an infection, which means that in order for it to appear in the body, infection must occur.
HPV penetrates the skin and mucous membranes of a healthy person upon their contact with the papillomas of a patient or with visually unchanged skin and mucous membranes of an infected person, provided that there is a large amount of virus at the site of contact and there is damage to the integrity of the epithelium (abrasions, scratches, wounds, erosions, sores). HPV infection is especially common in the presence of herpes simplex rashes, through which the human papillomavirus penetrates the skin and blood.
What to do if dangerous types of HPV are identified?
The risk of detecting dangerous types of HPV in an individual person is low.
In most people, no variant of this virus is detected at all.
If the patient is infected, then with a high probability it is a harmless type of HPV.
Low-oncogenic varieties are much more common.
If you are unlucky and have been diagnosed with highly oncogenic HPV, you need to look at its quantity.
If it is small, no treatment is required.
Most likely, your body has already begun to get rid of the virus, and soon it will no longer be detected.
It's worse if its concentration is high.
In this case, the following is necessary:
- additional tests;
- treatment;
- dynamic observation.
A smear is taken from the patient for oncocytology.
Most often, this study is carried out not after HPV genotyping, but simultaneously with this test.
Based on the results of these two tests, a decision can be made about the need for colposcopy.
It is needed to identify areas of altered epithelium (precancerous processes).
In turn, the results of colposcopy (examination of the cervix) may require a biopsy.
This is a procedure in which a piece of tissue is taken and sent for histological examination.
Based on its results, both a malignant tumor and a precancerous process of stages 1-3 can be diagnosed.
Stage 1 is reversible, while stages 2-3 require cauterization to prevent cancer.
But precancerous processes develop very slowly.
If antiviral treatment is carried out in time, the virus disappears from the body and the cervical epithelium is restored.
Patients must be monitored.
They are tested every six months to assess whether the concentration of the virus is increasing or decreasing.
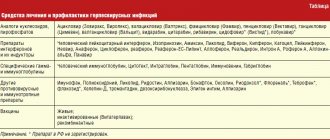
To eliminate it, antiviral and immunomodulating drugs are used.
How is the disease transmitted?
You need to know this in order to correctly prescribe a diagnosis. There are many ways of transmission. The virus can be located on any part of the skin or mucous membrane, that is, where there are epithelial cells.
The most common ways of transmitting the human papillomavirus are:
- Sexual vaginal contact.
- Anal sex.
- Oral sex (including cunnilingus) - possible infection of the pharynx and larynx with the development of oncology of these organs.
- Kiss in the presence of microtraumas of the mucous membrane.
- From mother to fetus as it passes through the birth canal.
- In case of close contact of damaged skin with papillomas of another person. The lesions may not be noticeable and often form during sexual contact in the pubic area, scrotum, and labia, which makes it possible to become infected with HPV when using a condom.
- Transfer of the virus from the surface of warts to damaged skin.
When is the material collected?
The method of collecting material for diagnosis and the material itself in general depend on the manifestations of human papillomavirus infection.
If there are elements on the skin and visible mucous membrane, then using a universal urogenital probe, a dermatovenerologist or gynecologist scrapes cells from the surface of the papilloma. The resulting cells are placed in a tube for delivery to the laboratory and PCR analysis for HPV. The manipulation is absolutely painless and takes about 30 seconds.
When diagnosing papillomavirus infection in the urethra, vagina, cervical canal, especially in the presence of cervical erosion, scraping is carried out from these organs, preferably from the erosion itself.
If papillomas are present on the mucous membrane of the oral cavity or rectum, then material is taken from these areas with a probe.
If it is necessary to diagnose diseases of the prostate gland or bladder, urine and prostate secretions can be taken for HPV.
Get tested for HPV in Moscow with us
To plan preventive methods, of course, HPV diagnosis is important.
You need to know whether you have this virus or not in order to understand the risks for sexual partners and the prospects for the development of this disease. Therefore, even if there are no manifestations, tests for papillomaviruses are necessary during a full examination by a urologist or gynecologist. Where you can get tested for HPV: daily from 10:00 to 21:00 in our clinics, seven days a week and on holidays. If necessary, you can get comprehensive advice on the diagnosis and treatment of human papillomavirus infection from experienced urologists, gynecologists and venereologists.